Base of Tongue Cancer
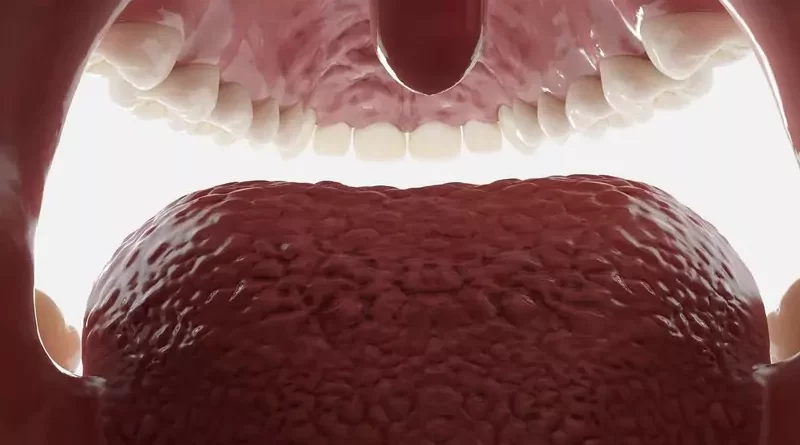
The base of tongue cancer is a type of throat cancer. These cancers are seen on the back of the tongue, where the tongue connects to the throat. The most common type of these cancers is base of tongue squamous cell carcinoma. Squamous carcinoma originates from thin, flat squamous cells covering the surface of the tongue.
Tumor on the base of the tongue develops from the back one-third part of the tongue. The exact cause of base of tongue cancers is unknown. Tobacco use, alcohol consumption, human papillomavirus infection, and weakened immune system are important risk factors for the formation of base of tongue cancers. The base of tongue cancer shows signs and symptoms in the late stages. Avoiding some risk factors is very crucial for the base of tongue cancer prevention.
The diagnosis of the base of tongue cancer can be made by biopsy. Response to treatment and survival rate may vary depending on the association of base of tongue cancer with human papillomavirus (HPV) or tobacco-alcohol and the age of the patient. The main treatments for the base of tongue cancers are surgery, radiation therapy, and chemotherapy. TransOral Robotic Surgery for the base of tongue cancer is also a surgical option. Brachytherapy, targeted therapy, and immunotherapy are added to the treatment as needed.
Signs and Symptoms
The base of tongue cancers develops from the back one-third part of the tongue, where it connects to the throat. The base of tongue cancer shows signs and symptoms later than oral tongue cancers. The time of detection is either the regular exam or the moment when they give symptoms. Because they are not in an easily visible place in the mouth. Therefore, the base of tongue cancer is usually at the late stages when the doctor diagnoses them.
Lump in the neck
The base of tongue cancer, while still small and quiet, spreads to lymph nodes in the neck over time. Therefore, swollen lymph nodes can sometimes be the first sign of the base of the tongue.
Persistent sore throat
Pain is one of the first symptoms of the base of tongue cancers, as they are not in a visible place and the patients can not notice their occurrence in the early period. Pain presents itself in the form of a persistent sore throat. This pain hits the ear on the affected side, causing ear pain on one side over time. In terms of base of tongue cancer, sore throat and ear pain on one side can be serious symptoms.
The feeling of something stuck in the throat
As the base of tongue cancer progresses and grows, the patient will experience the feeling of something stuck in the throat. The patient feels pain when speaking and difficulty in swallowing. In particular, in the base of tongue cancers, hoarseness and changes in voice are also seen.
Persistent ulcers in the throat
The HPV-associated base of tongue cancer starts in the grooves of the back of the tongue. HPV usually does not give any symptoms until it causes the base of tongue cancer. When it shows symptoms, it usually presents itself with ulcers in the throat and on the back of the tongue and also swelling in the neck area. The base of tongue cancer usually spreads to lymph nodes in the neck in the early stages.
In summary, signs and symptoms of the base of tongue cancer may include:
Lump in the neck
Swelling in the neck area
Persistent sore throat
The feeling of something stuck in the throat
Persistent ulcers in the throat
Persistent throat infections
Difficulty swallowing solid foods
Pain while speaking
Hoarse voice
Ear pain on one side
Jaw stiffness and pain
Unexplained weight loss
Blood in spit
Halitosis
Causes
The exact cause of the base of tongue cancer is unknown. However, several well-known factors have an impact on the development of the base of tongue cancer. These factors are mainly all kinds of tobacco use, excessive alcohol consumption, sexually transmitted Human Papillomavirus infections, and a weakened immune system. Recently, the role of Human Papillomavirus (HPV) in the occurrence of the base of tongue cancer has increased with the change of sexual behaviors. Today, most of the base of tongue cancers are HPV-related, except for a small number of them.
Risk Factors
The base of tongue cancers of older men with more comorbidities are generally associated with tobacco-alcohol use. However, human papillomavirus (HPV) -related base of tongue cancers are more common in both genders and younger ages. People with HPV-related base of tongue cancers have short-term or little or no tobacco-alcohol use. The base of tongue cancer can also develop in HPV-negative elderly and young people who do not use tobacco and don’t drink alcohol.
Tobacco and alcohol use
The two most important independent factors for the development of the base of tongue cancer are tobacco and alcohol use. Tobacco smoke contains several known carcinogenic substances, mainly nitrosamines. Alcohol turns into acetaldehyde, adversely affecting DNA repair. Especially if there are tobacco use and alcohol consumption, and the two are together, the risk of the base of tongue cancer is higher. Tobacco and alcohol use are the causes mostly seen in elderly patients.
Human papillomavirus infection
Human papillomavirus (HPV) is a sexually transmitted virus. HPV can lead to cancer development in the genital area, mostly in women. Apart from this, HPV can cause penile cancers in men and anal cancers. There are many types of HPV. Especially high-risk types 16 and 18 can lead to tumor development in both the genitals and the tongue, mouth, throat. HPV mainly plays a role in the development of the base of tongue cancer. Oral tongue cancers are generally not HPV-related.
Due to various sexual behaviors, the prevalence of HPV-associated base of tongue cancers in teenagers has increased in recent years. Especially types 16 and 18 HPV are present in many cases associated with the base of tongue cancers. Normally, the immune system can often eradicate even high-risk types of HPV within months to years. But in people with weakened immune systems, the virus can take advantage of this and cause cancer.
A weakened immune system
Immunodeficiency, being an organ transplant recipient, and treatments that suppress the immune system are also factors that have an impact on the occurrence of the base of tongue cancer. The presence of base of tongue cancer in people who are HPV-negative, who do not have tobacco and alcohol use, may be associated with a weakened immune system.
In summary, factors that may increase the risk of the base of tongue cancer include:
All forms of tobacco use
Excess alcohol consumption
Human papillomavirus infection
A weakened immune system
Being an organ transplant recipient
Immunosuppressive therapy
Immunodeficiency
Poor oral hygiene
Being elderly male
Environment
Genetic factors
Types of Tumors
A tumor on the base of the tongue often refers to a malignant tumor. The base of tongue cancer usually spreads rapidly and metastasizes to lymph nodes in the neck. Most of these cancers are squamous cell carcinomas and the remaining few are malignant minor salivary gland tumors. In rare cases, there may be metastatic cancers of the base of the tongue.
Squamous cell carcinoma
The most common malignant tumor on the base of the tongue is squamous cell carcinoma. Squamous cell carcinoma develops from squamous cells, which are thin and fat cells in the epithelial layer lining the inner parts of the body. Squamous cell carcinoma is also a common type of cancer in the nose, mouth, throat, pharynx, and larynx. The HPV-associated base of tongue cancer is also a type of squamous cell carcinoma.
Minor salivary gland tumors
The second most common malignant tumor on the base of the tongue is minor salivary gland tumors. These are mucoepidermoid carcinoma, adenocarcinoma, and adenoid cystic carcinoma, which are minor salivary gland-derived malignant tumors.
Diagnosis
The patient who suspects base of tongue cancer should first consult an ear, nose, and throat doctor (otolaryngologist). For the diagnosis of the base of tongue cancer, the doctor first examines the patient’s mouth, throat, and neck. Then, the doctor takes tissue samples from the suspicious areas of the base of the tongue for examination by the pathologist. Necessary imaging tests are also performed to aid diagnosis.
Physical exam
The doctor first listens to the patient’s complaints and then examines the mouth, throat, and neck. Tonsils and the back of the tongue may require examination with special devices. The doctor examines the base of the tongue with a special device called an endoscope and the patient’s voice box with a laryngoscope. The doctor then examines the lymph nodes in the neck and checks for a lump or swelling in the neck area.
Removing a tissue sample
The doctor takes tissue samples from the suspicious parts of the base of the tongue. The tissue sample is taken from the lump in the neck with a thin biopsy needle. The doctor takes a tissue sample from the patient (biopsy) under local anesthesia, if necessary, and without causing excessive bleeding. Examination of these tissue samples by the pathologist is necessary for the diagnosis of the base of tongue cancer. The biopsy is not a procedure that will lead to the spread of the base of the tongue tumor.
Imaging tests
To investigate whether the tumor on the base of the tongue has spread to surrounding tissues, the patient’s head and neck region are examined by imaging tests such as ultrasonography (USG), computerized tomography (CT), or magnetic resonance imaging (MRI). Positron emission tomography (PET) is important to investigate the spread of the base of tongue tumors to distant regions.
Treatment
The treatment of base of tongue cancers includes surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. There may be different treatment combinations depending on the type of cancer, its relationship with HPV, its stage, spread, general health status, and preference of the patient.
Surgery is usually the first treatment for the tobacco-alcohol-related base of tongue cancers. Radiation therapy and chemotherapy are added to surgery when necessary. Radiation therapy and chemotherapy combination (chemoradiation) are at the forefront for HPV-related base of tongue cancers. Because HPV-associated base of tongue cancers respond better to chemoradiation.
Chemoradiation is also the first choice for HPV-related base of tongue cancers because it affects speech and swallowing less than surgery. In cases where surgery is not possible for various reasons, chemoradiation can replace it. But in general, surgery is still effective at many stages of the base of tongue cancers. Treatment of base of tongue cancer may also include targeted therapy and immunotherapy as needed.
Treating doctors
Generally, otolaryngologists experienced in head and neck surgery perform the surgical treatment of base of tongue cancers. In addition to surgical treatment, radiation oncologists deliver radiation therapy, and medical oncologists deliver chemotherapy. Plastic surgeons, dentists, psychiatrists, speech, nutrition, swallowing, and pain management specialists can also participate in the treatment of base of tongue cancer.
Surgery
Surgery is usually the first choice in the treatment of tobacco-alcohol-related base of tongue cancers. Because in these cases, the applicability and efficiency of surgery are more. Since the base of the tongue is surgically difficult to reach orally, TransOral Robotic Surgery (TORS) can provide an advantage in surgery. However, TransOral Robotic Surgery is mainly advantageous in the surgery of early-stage base of tongue cancers. In the treatment of late-stage base of tongue cancers, if HPV-negative, traditional surgery is the first choice. In the treatment of HPV-related late-stage base of tongue cancers, the main preference is chemoradiation.
Tumor removal
The surgeon decides how to remove the tumor based on preoperative examination and imaging tests. The surgeon removes the tumor on the base of the tongue by an incision in the neck or through the mouth, depending on its size or spread to surrounding tissues. The base of tongue cancers is usually in the late stages when diagnosed. In this respect, the surgeon can remove part or all of the tongue (glossectomy). Apart from that, if cancer has spread to the voice box (larynx), there is a possibility of removal of the voice box (laryngectomy). To make sure that no cancerous tissue is left behind, the surgeon removes the tumor on the base of the tongue along with some healthy tissue around it.
Incision into the windpipe
For the patient to breathe comfortably or in cases where the tubes extended from the mouth to the windpipe make the surgery difficult, the surgeon makes a hole into the windpipe from the anterior part of the neck (tracheotomy). By placing a tube in this hole (tracheostomy), the patient breathes during anesthesia. Thus, the surgeon secures the patient’s airway during and after surgery. After the patient begins to heal and the swelling (edema) in the surgical area has passed, this hole is closed.
Lymph node removal
During the surgery of base of tongue cancers, the surgeon also removes some lymph nodes by incision from the neck (neck dissection). The surgeon determines which of the neck lymph nodes to be removed, according to examination, biopsy, imaging tests, and also his own preference. In particular, the surgeon removes lymph nodes in the neck that are likely to contain metastases. Usually, the base of tongue cancers has already spread to the lymph nodes at the time of diagnosis. Even if no metastases are detected in the examination and imaging tests, the surgeon performs the neck dissection as a precaution against future neck metastases.
Reconstruction
After removing the base of the tongue tumor, the surgeon takes tissue samples for control purposes from adjacent parts of the removed area. After the pathologist reports these tissue samples as cancer-free, the surgeon goes to the repair stage. If the amount of tissue removed with the tumor is small, the surrounding tissues will be sufficient for repair. Otherwise, the surgeon may move tissue from distant parts of the body such as the anterior chest wall, hips, legs, as needed, for repair. In this way, the surgeon repairs the gaps and then closes the incisions.
Normalization process after surgery
After surgery, the patient spends a few days in the hospital. The patient may spend some of this time in intensive care. Over time, the patient gets rid of drains, tubes, and catheters that expel blood and fluid accumulations from the surgical wound. During this period, the doctor also removes the patient’s tracheotomy cannula, if any. After surgery, the patient feeds with a tube extending from the nose to the stomach or with special nutritional fluids from the vein for a while. To prevent infections and relieve pain, the patient also takes antibiotics and pain relievers intravenously.
After a while, the surgical wounds of the patient’s mouth and throat heal. The surgeon then closes the windpipe hole in the patient’s neck, if present. Then, the patient begins to feed with liquid and soft foods orally. After the patient can make a sound, speak and eat normally, the hospitalization period of the patient ends.
Radiation therapy
Radiation oncologists use radiation therapy with a radiation device to destroy cancer cells. Before this treatment, the patient must recover after tongue surgery. In cases where surgery is not possible for various reasons, the patient receives radiation therapy for the regression of the base of tongue cancer. Radiation therapy is often combined with chemotherapy (chemoradiation). Since HPV-related base of tongue cancers respond well to radiation therapy, radiation therapy can be an alternative to surgery. In particular, radiation therapy does indeed have benefits in the treatment of late-stage HPV-related base of tongue cancers and in preventing recurrence of cancer.
Brachytherapy
Brachytherapy is a type of radiation therapy. In brachytherapy, the radiation oncologist places small tubes containing radioactive material around the base of the tongue tumor for a certain period of time. Brachytherapy is one of the treatments in cases where the base of tongue cancer still exists after surgery and radiation therapy.
Chemotherapy
Medical oncologists administer chemotherapy by giving the patient anti-cancer drugs. Anti-cancer drugs reach cancer cells that have spread throughout the body through the bloodstream. Chemotherapy is an additional treatment to radiation therapy in the treatment of base of tongue cancers. Chemotherapy particularly increases the effectiveness of radiation therapy to which HPV-related base of tongue cancers respond well.
Targeted therapy
Medical oncologists often combine targeted therapy with chemotherapy in the treatment of base of tongue cancers. Targeted therapy is treatment with drugs and substances that mainly target cancer cells. Targeted therapy does less damage to healthy cells. Therefore, the side effects that occur during targeted therapy are milder than chemotherapy. The effects of targeted therapy drugs are also different from chemotherapy drugs.
Immunotherapy
A medical oncologist also treats cancer using immunotherapy. Cancer cells make the immune system cells dysfunctional against cancer with some proteins they produce. In these situations, the immune system needs powerful stimulants that strengthen it. Immunotherapy aims to make the immune system more active. Immunotherapy may be an option in cases where cancer progresses and other treatments are not an option.
Vocal functions after surgery
The organ that creates sound in the body is the larynx (voice box). The pharynx, palate, tongue, and lips use the raw sound of the larynx for the pronunciation of letters and words. Surgery of the larynx area affects vocal functions. Placing the tube in the windpipe by incision seriously affects the vocal functions of the patient. Except for the removal of the voice box (laryngectomy) due to the spread of the base of tongue cancer to the larynx, the patient starts to make a sound easily after the tracheotomy hole in the neck is closed.
Speech functions after surgery
Our tongue and mouth play an important role in the pronunciation of letters and words. Surgeries in these areas affect the patient’s speech function. After the surgical wounds on the tongue, mouth, and throat of the patient heal, the speech can be understood more easily. However, language has an important role in the pronunciation of some letters. For this reason, the pronunciation of these letters may be less clear after the base of tongue cancer surgery. If such pronunciation problems are severe after surgery, voice and speech therapists can assist the patient.
Taste functions after cancer treatment
There is not much deterioration in taste after the base of tongue surgery. Since the patient cannot feed orally in the first days after the surgery, it is not possible to taste. However, if the patient has also received radiation therapy, there may be taste disturbances for a while. Radiation therapy can also cause dry mouth, due to its side effects. In these cases, ADA approved mouth moisturizers (eg, Biotene Dry Mouth Oral Rinse, or as a different choice: TheraBreath Dry Mouth Oral Rinse, etc.) may be beneficial.
Feeding after surgery
Depending on the size of the base of tongue cancer surgery, the patient cannot feed orally for a while after the surgery. During this period, the patient feeds with special nutritional fluids through a tube extending from the nose to the stomach or intravenously. After the surgical wounds in the mouth and throat are healed and the hole in the windpipe is closed, the patient begins to feed with liquid and soft foods orally. In the following days, the patient can feed normally. After the removal of a tumor on the base of the tongue, swallowing problems may develop in the patient. However, some successful surgical procedures can alleviate or eliminate these problems.
Prognosis
The success rate of the base of tongue cancer treatment depends on the type of tumor, its relationship with human papillomavirus (HPV), its stage, and how far it has spread. The chance of success in the treatment of base of tongue cancer in the early stages is quite high. Since they are generally detected in late stages, survival rates may decrease according to the spread of cancer.
The HPV-related base of tongue cancer tends to appear at a younger age and respond well to existing treatments, especially chemoradiation. But HPV-negative base of tongue cancer is cancer of older patients. Therefore, HPV-negative base of tongue cancers in this group of patients has a relatively poor prognosis. However, treatment of base of tongue cancer is still possible in many cases.
Follow-up care
Although the patient has received all the treatments, there is a risk of recurrence of the base of tongue cancer. The first years after surgery is the period when the possibility of recurrence of the base of tongue cancer is the highest. Over the years, this possibility decreases. The patient comes for regular controls for up to 5 years after cancer treatment. These checks are necessary for the doctor to detect if cancer recurs. Recurrence of the base of tongue cancer after the fifth year is considered new cancer, not a comeback.
Recurrence of the base of tongue cancer
The recurrence of the base of tongue cancer is not the end of everything. In case of recurrence of the base of tongue cancer, the doctor will investigate whether he can perform surgery again. If the base of the tongue’s cancerous tissue can be completely removed, the surgeon can perform surgery again. Additional surgery is still possible if the patient has previously received only radiation therapy and chemotherapy.
In cases where repeat surgery is not possible, additional doses of radiation therapy come to the fore. However, there is also a reality that a full dose of radiation therapy is effectively applied to an area, usually only once. Therefore, the patient receives one more radiation therapy, this time at a lower dose, to the tumor area. Brachytherapy is also one of the options in such cases. In addition, in cases of recurrence of the base of tongue cancer, the patient can receive chemotherapy repeatedly as long as the immune system lifts it.
Prevention
Stop tobacco use
To reduce the risk of developing base of tongue cancer, a person should avoid all types of tobacco use, including smoking and chewing. Tobacco use is a factor that may also affect the recurrence of the base of tongue cancer. To reduce all these risks, the patient should stop tobacco use, if any. If quitting tobacco is not easy for the patient, the help of a psychiatrist or psychologist can be effective.
Stop or limit alcohol intake
Alcohol also has an effect on the occurrence or recurrence of the base of tongue cancer. To reduce these risks, the person should stop drinking, if any. If it is not easy to quit alcohol, one should at least limit alcohol use. Rehab centers can help you find ways to quit alcohol.
In addition, even the use of alcohol-containing oral care products is also risky. Because they regularly expose the mouth to alcohol. That is why, the use of alcohol-free products (eg, ADA approved mouthwash: TheraBreath Fresh Breath, CloSYS Sensitive Gentle Mint, CloSYS Ultra Sensitive Unflavored, or as a different choice: Tom’s of Maine Natural Wicked Fresh, etc.) is safer.
Prevent human papillomavirus infection
The role of human papillomavirus (HPV) in the development of the base of tongue cancer has increased. Safe sexual intercourse is important to prevent sexually transmitted HPV. It is important to remember that HPV infection can also occur during oral sex. In this respect, condoms are not enough to protect against HPV. Getting a full course of HPV vaccine can also reduce the risk.
Have regular checkups
The base of the tongue is not in a place that can be easily seen from the mouth. Accordingly, the base of tongue cancers usually shows themselves when they give symptoms. In this respect, regular checkups increase the possibility of detecting the base of tongue cancer at an early stage.
Live a healthier life
HPV-negative people who do not use tobacco and do not consume alcohol can also get base of tongue cancer. In these cases, lifestyle becomes important. In this respect, it is necessary to eat a healthy diet, exercise regularly, practice good oral hygiene, keep immunity and morale high.
References
American Cancer Society: “Risk Factors for Oral Cavity and Oropharyngeal Cancers”
American Cancer Society: “Surgery for Oral Cavity and Oropharyngeal Cancer”
National Center for Biotechnology Information (NCBI): “Tongue Cancer”
NCCN Clinical Practice Guidelines in Oncology: “Head and Neck Cancers, Version 2.2020”
Penn Medicine: Throat (Oropharyngeal) Cancer, “Types of Throat (Oropharyngeal) Cancer”
UT Southwestern Medical Center: Condition and Treatments, “Base of Tongue Cancer”