Hard Palate Cancer
The hard palate is the anterior bony portion of the roof of the mouth. It is a part of the oral cavity and cancers can develop from here. The most common type of cancer is squamous cell carcinoma of the hard palate. Hard palate squamous cell carcinoma develops from the thin, flat squamous cells lining the mucosal surface of the bone (periosteum) here.
The exact cause of hard palate cancer is unknown. Tobacco use, alcohol consumption, precancerous lesions, and weakened immune system are the main risk factors for the formation of hard palate cancers. Hard palate cancers usually give signs and symptoms in the early stages. Avoiding risk factors is beneficial in hard palate cancer prevention.
The diagnosis of hard palate cancer can be made by biopsy. The survival rate may vary depending on the type, stage, and spread of the hard palate cancer. Generally, the main treatments for hard palate cancer are surgery, radiation therapy, and chemotherapy.
Hard Palate
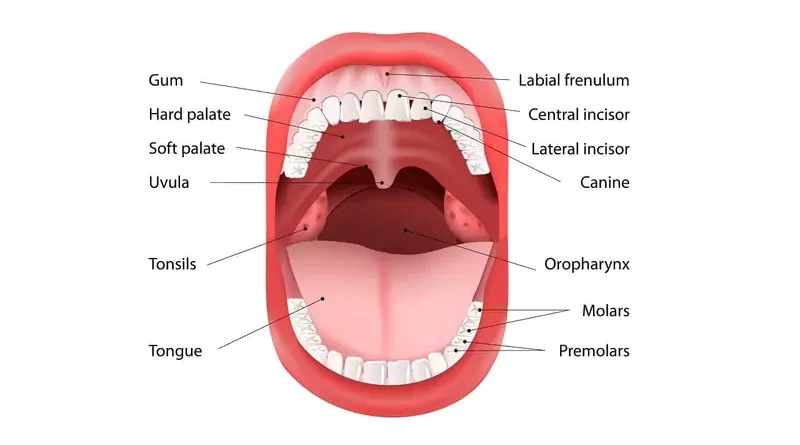
The hard palate is the bony front portion of the roof of the mouth. There are teeth on the front and sides of the hard palate, and the soft palate and uvula behind it. The hard palate separates the oral cavity from the nasal cavity and the maxillary sinuses. Hard palate cancers may spread into the nasal cavity and the sinus when they become more advanced.
Most hard palate tumors are malignant but they are less common than other cancers of the head and neck region.
Signs and Symptoms
Hard plate cancers are uncommon malignant tumors. Some benign lesions can also mimic hard palate cancers and need to be distinguished. One of them, torus palatina, the bony growths of the palate are hard midline masses that produce no symptoms. So they should not be confused with hard palate tumors.
Ulcer on the roof of the mouth
The main symptom of tumors developing from the hard palate is a raised or flat color change or ulcer on the mucosal surface that has been present for more than 2-3 weeks. The most common sign of hard palate cancer is an ulcerated wound on the roof of the mouth. As cancer grows, the ulcer may bleed.
Swelling of the roof of the mouth
Some hard palate cancers present themselves as swelling under the mucosa, that has been present for more than 2-3 weeks, rather than an open wound or ulcer. Especially minor salivary gland tumors cause submucosal lesions with a smooth, normal mucosal covering on the hard palate.
Numbness or pain in the upper jaw
Often, the cancer is asymptomatic in the early stages, but patients may experience pain in advanced stages. As the hard palate tumor grows and invades deep tissues such as muscle, nerve, or bone, pain, and difficulty in chewing and swallowing occur. Hard palate cancer may cause numbness in the face along with pain which could make speaking difficult.
Loose teeth or ill-fitting dentures
There may be additional symptoms in patients with hard palate cancer such as loose teeth or dentures that no longer fit in. Losing teeth occur if cancer invades the bone or the tooth sockets in which the teeth are rooted. Also, if there is dental numbness, it may indicate nerve invasion of cancer.
Lump in the neck
Hard palate tumors can spread to lymph nodes in the neck and cause swelling there. Approximately one-third of patients have neck lymph node metastasis at the time of exam. That is why, in some cases, the first sign of hard palate cancer could be a lump in the neck. However, patients notice hard palate cancers usually before it reaches these lymph nodes.
Other symptoms
A patient with hard palate cancer may also have a foul odor in the mouth. Apart from this, in an advanced stage, hard palate cancer, spasm of the jaw muscles, or neck mass may cause the mouth to remain tightly closed. However, since the hard palate area is easily visible, the patient himself, the dentist, or the doctor usually detect the tumors in the early stages.
Causes
Currently, there is no exact cause of hard palate cancer. However, tobacco use and alcohol consumption contribute to the development of hard palate cancers. Genetic and other environmental factors are likely to have a combined effect in the development of hard palate cancer, as in other cancers.
Human papillomavirus (HPV) infection can lead to the development of cancers of the tonsil, base of the tongue, and sometimes soft palate. However, the opinion that HPV does not play a role in hard palate cancers is common among experts dealing with this issue.
Risk Factors
All kinds of tobacco use
Tobacco is the biggest contributing factor to hard palate cancers. Especially, in the case of reverse smoking (the lit end of the cigarette is placed in the mouth), the risk increases more. There are suspicions that the intense heat generated during reverse smoking is a carcinogen. Also, we know that chewing betel (the seed of the areca tree) also causes hard palate cancer.
Alcohol consumption
Alcohol consumption is a serious risk factor for cancer of the hard palate. There is a strong relationship between excessive alcohol consumption and the onset of oral squamous cell cancers. Moreover, smoking and drinking heavily more than doubles hard palate cancer risk.
Being older male
Hard palate cancers are more common among elderly people, especially after the fifth decade. People with hard palate cancer are mostly men.
Other risk factors
There are other risk factors for developing hard palate cancer also. Weakened immunity, ill-fitting dentures, poor oral hygiene, marijuana use, and vitamin deficiency may also be associated with hard palate lesions.
Types of Tumors
Similar to other parts of the body, the uncontrolled growth of cells covering the hard palate or in other underlying tissues causes cancer. The most common malignant tumors of the hard palate are squamous cell carcinoma, minor salivary gland cancers, mucosal melanoma, Kaposi sarcoma, and non-Hodgkin lymphoma. Half of all hard palate cancers are squamous cell carcinomas. Other hard palate cancers account for the other half.
Squamous cell carcinoma
Squamous cell carcinoma is the most common malignancy in the oral cavity. It remains the most common malignant lesion in the hard palate, with a predilection for male patients in their 6th decade. Squamous cell carcinoma of the hard palate usually starts on the surface of the tissues (mucosa). Lymph node involvement is high in squamous cell carcinomas.
Minor salivary gland cancers
Salivary gland cancers such as adenoid cystic carcinoma, mucoepidermoid carcinoma, and adenocarcinoma can also develop from minor salivary glands, which are highly concentrated in the hard palate mucosa. Lymph node involvement is of special concern in high-grade mucoepidermoid carcinomas. It is rare in other salivary gland carcinomas. The exact cause of minor salivary gland malignancies remains unknown.
Mucosal melanoma
Mucosal melanoma comprises a rare but aggressive form of hard palate cancers. They are one of the soft palate cancers, are smooth black, brown, or brownish-gray lesions. The causes of mucosal melanoma of the hard palate are unclear.
Kaposi sarcoma
Kaposi sarcoma is associated with immunosuppression. It is linked to the human herpesvirus 8 (HHV8) and human immunodeficiency virus (HIV). The lesions are bluish in color in Kaposi’s sarcomas, which are common in HIV-positive patients.
Non-Hodgkin lymphoma
Non-Hodgkin lymphomas may arise in the oral cavity, commonly at the junction of the hard and soft palate. The risk factors for developing non-Hodgkin lymphoma are mainly multifactorial such as are immunosuppression, viral infections, tobacco use, occupational toxin exposure, etc.
Benign hard palate tumors
Neurofibroma, neurilemmoma, lipoma, leiomyoma, and benign minor salivary gland tumors (pleomorphic adenoma, basal cell adenoma, myoepithelioma, and cystadenoma) can also develop from the hard palate.
Diagnosis
The patient who suspects hard palate cancer should first consult an ear, nose, and throat doctor (otolaryngologist). The diagnosis begins when the patient, who notices the persistent ulcer or swelling on the roof of the mouth, consults a doctor. Generally, the doctor takes a detailed history including pain symptoms, the time of formation of the palatal mass, growth rate, and prior oral trauma if any. Then the doctor proceeds to the examination phase.
Physical exam
Physical examination includes a comprehensive head and neck exam with a focus on the oral cavity. The doctor palpates neck lymph nodes bilaterally. After the examination, if the doctor suspects the presence of a hard palate tumor, he/she may need various imaging tests (such as MRI, CT, PET) and tissue samples from the suspicious area of the patient’s hard palate.
Removing a tissue sample
If the doctor examining the patient considers the hard palate lesion suspicious enough, tissue samples are taken from the lesion (biopsy). The doctor takes the tissue sample from the hard palate tumor, under local anesthesia, by making a small incision or removing a small piece from the lesion. Biopsy does not cause the spread of hard palate tumors and is necessary for diagnosis.
The pathologist examines the tissue samples taken from the hard palate in detail under the microscope and makes the diagnosis of the tumor. Examination of the lesion under local anesthesia and biopsy can provide additional information regarding the extent of the palatal tumor.
Imaging tests
The otolaryngologist who examines the hard palate may request magnetic resonance imaging (MRI) or computed tomography (CT) imaging tests, if necessary. Although positron emission tomography (PET) has a poor resolution, it is superior in detecting distant metastases and post-treatment surveillance. Imaging tests can be done before or after a biopsy. These tests contribute to treatment planning in terms of showing the spread and stage of the hard palate tumor.
Treatment
Specific treatment of palate cancer depends on the location, stage, and type of the malignant tumor. In general, the main treatment for cancers developing in the hard palate area is surgery. If the hard palate cancer is more advanced, radiation therapy, chemotherapy, or both (chemoradiation) may be used to shrink the tumor before or after surgery. Chemoradiation reduces the risk of cancer coming back. For some people, radiation therapy may be the sole treatment.
Treating doctors
Mainly, otolaryngologists, experienced in head and neck surgery or oral and maxillofacial surgeons undertake the diagnosis, treatment planning, and surgical treatment of hard palate cancers. When necessary, radiation oncologists for radiation therapy and medical oncologists for chemotherapy are included in the treatment process. Depending on the need, plastic reconstructive surgeons, dentists, speech-language pathologists, psychologists, and other health professionals can also participate in the process.
Surgery
Surgery is often the first step in the treatment of hard palate cancers. The choice of the surgical technique is based on the location and size of the palatal tumor. The surgeon usually performs the surgery via a transoral approach without the need to use facial incisions. However, the external approach may also be necessary for very advanced tumors.
Studies have shown that surgery for hard palate cancers provides higher disease-free survival compared with non-surgical treatments. Furthermore, hard palate tumors tend to display early invasion to the underlying bone (periosteum), which is not very responsive to radiation therapy.
Tumor removal
The main purpose of surgical treatment is to remove all cancerous tissues on the hard palate without leaving tumor cells behind. In this respect, the surgeon removes the cancerous tissue in the hard palate with adequate safety margins.
The bone closest to the hard palate tumor often contains cancer cells. This requires the removal of some healthy hard palate tissues surrounding the tumor. That is why an operation called a maxillectomy is often part of the hard palate tumor treatment. Maxillectomy is the surgical removal of a part of the whole upper jawbone as treatment.
Lymph node removal
During surgery, the surgeon removes the lymph nodes (neck dissection) with a high probability of cancer spreading in the neck. Especially, squamous cell carcinoma and high-grade mucoepidermoid carcinoma of the hard palate should be treated aggressively. So in these cases, the surgeon performs neck dissection because of the high rate of lymph node metastasis. Neck dissection is one-sided for tumors that do not involve the palatal midline. In case of tumors involving the midline, the surgeon performs bilateral neck dissection.
Restoration
If the tumor is small, the surgeon closes the removed area by using surrounding tissues or tissue transfer. If the removed area is large, the surgeon uses a prosthesis to cover the opening in the roof of the mouth. The prosthesis is well tolerated during radiation therapy and permits visualization of cancer recurrence. The palatal prosthesis looks similar to a denture plate.
Restoration of function to the hard palate region is vitally important. Because most cancer surgeries in the palatal region involve an opening in the palate and maybe a loss of some of the upper teeth. Free tissue transfer is an option for larger palatal defects. Therefore, soft palate restoration may require a second surgical team.
Normalization after surgery
After surgery for a hard palate tumor, the patient can stay in intensive care for a few days. During the hospitalization, the patient takes antibiotics against infections, pain relievers, and other necessary medications. The patient carries over the drain, which drains fluid and blood from the surgical site for a while.
During this period, the patient feeds by a tube that extends from the nose to the stomach. After the patient can feed orally and speak, the hospitalization period of the patient ends.
Radiation therapy
Radiation therapy is the treatment of tumors by giving radiation with special devices. Today’s radiation devices can be directed to the tumor with the least damage to the healthy tissues around the tumor. Radiation therapy shrinks or eliminates tumors by destroying cancer cells.
Radiation therapy is a post-surgical treatment of choice if the malignant hard palate tumor could not completely be removed or it was determined to be aggressive or had spread to lymph nodes, nerves, vessels, etc.
Radiotherapy is usually an additional treatment after surgery for hard palate cancers. However, in some cases, complete surgical removal of a hard palate cancer may be impossible because of its size or extent of involvement or unsafe. Radiation therapy is a primary treatment option in these cases. But, radiation therapy is ineffective for malignant salivary gland tumors of the hard palate due to their radioresistance and frequent bony invasion.
Chemotherapy
Chemotherapy is an adjunct to radiation therapy and enhances its effect. Together with radiation therapy (called chemoradiation), it may be an alternative to surgery. Especially, non-Hodgkin lymphoma of the hard plate is primarily treated with chemoradiation. But other than that, the usage of chemotherapy is not common in the treatment of hard palate cancers.
Targeted therapy
Nowadays, as a result of the developments in the pharmaceutical industry, targeted therapy, which is a more advanced type of chemotherapy, has started to gain importance. Although targeted therapy is still at an early stage in cancer treatment, expectations are high.
Speaking and swallowing after tumor surgery
Depending on the scope of palate surgery, repair method and additional postoperative treatments, some impairment in speech and swallowing may occur after surgery. However, there are also successful surgical procedures that will alleviate or eliminate swallowing and speech problems that may develop in patients after the hard palate tumor is surgically removed.
Feeding after tumor surgery
The patient feeds through a tube extending from the nose to the stomach or intravenously during hospitalization. But over time, the patient starts feeding orally. Patients need to regain some pre-treatment feeding function to prevent malnutrition and aspiration.
Taste functions after cancer treatment
After hard palate tumor surgery, there is not much deterioration in taste. However, if the patient has received radiation therapy in addition to surgical treatment, there may be taste disturbances. Radiation therapy can also cause dry mouth in the patient due to its side effects. In these cases, ADA approved mouth rinse (eg, Biotene Dry Mouth Oral Rinse, or as a different choice: TheraBreath Dry Mouth Oral Rinse, etc.) may be beneficial for the patient.
Prognosis
The survival rate in hard palate cancers depends on mainly early diagnosis, type of tumor, and appropriate management. Early diagnosis allows minimal treatment with less morbidity and better survival chances. The exact site of the hard palate cancer and bone invasion does not have much impact on the survival outcome. Prognostic factors of hard palate cancer are mainly the stage of cancer, lymph node metastases, and resection margins.
Follow-up care
Recurrence of hard palate cancer can often occur many years after initial treatment. Therefore, continuous follow-up is very important. According to the guidelines for post-treatment surveillance, patients should receive regular follow-up several times a year in the first 5 years after treatment and once a year after the 5th year.
The recommended follow-up for these malignancies is over 10 years. The importance of long-term follow-up is crucial for several hard palate malignancies because of their high recurrence rates and indolent growth patterns.
Recurrence of hard palate cancer
Hard palate malignancies can come back several years, even decades, after initial treatment. Recurrence of hard palate cancer after treatment does not mean that there are no treatment options. Even in the case of recurrence, the prognosis is good in terms of survival. Depending on the extent of previous treatment and the spread of recurrent hard palate cancer, the doctor reviews appropriate treatment options such as repeat surgery, radiation therapy, and chemotherapy.
Patients may develop depression and social anxiety due to cancer come-back. Consultation with support groups and a psychologist can help patients relieve their anxiety.
Prevention
Don’t use tobacco
Patients who receive surgical and non-surgical treatments for hard palate cancer should definitely stop tobacco, if any, to minimize the possibility of recurrence of the disease.
Limit alcohol consumption
The person should stop or limit alcohol consumption if any. Limiting alcohol intake reduces the risk of occurrence, recurrence of hard palate cancer, and poor treatment outcomes. Even the use of alcohol-containing oral care products is risky in terms of regularly exposing the mouth to alcohol. So, the use of alcohol-free products (eg, ADA approved mouthwash: TheraBreath Fresh Breath, CloSYS Sensitive Gentle Mint, CloSYS Ultra Sensitive Unflavored, or as a different choice: Tom’s of Maine Natural Wicked Fresh, etc.) is very important.
Get the regular dental care
Dentists are typically the first to notice hard palate cancer, often during routine dental exams. Regular dental checkups are important for the early detection of hard palate cancer.
Live a healthy life
Oral hygiene, a healthy diet, and keeping morale high are important factors in reducing the risk of developing all types of oral cancers, including hard palate cancer. It is also important that patients who have received treatment have their follow-up, examination, and tests regularly.
References
Memorial Sloan Kettering Cancer Center: Mouth Cancer, “Hard palate cancer”
National Center for Biotechnology Information (NCBI): “Malignant tumors of the hard palate: Report of 4 cases and review of the literature”
NCCN Clinical Practice Guidelines in Oncology: “Head and Neck Cancers, Version 2.2020”
PubMed, Journal of Oral and Maxillofacial Surgery: “Neoplasms of the hard palate”
StatPearls: “Malignant Tumors of the Palate”