Tonsil Cancer
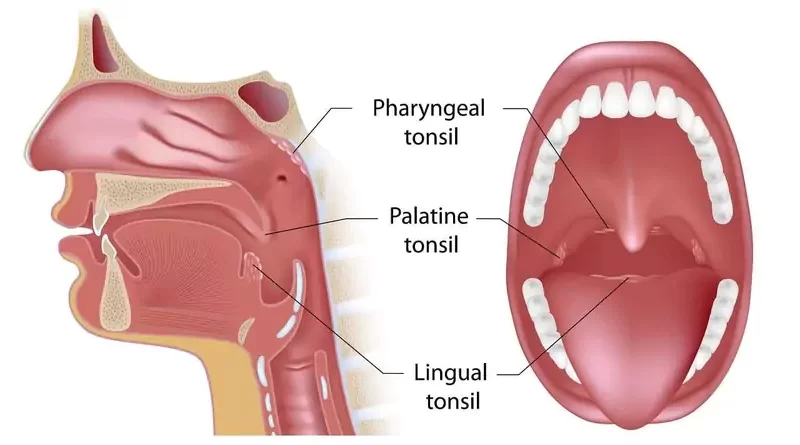
Tonsil cancer is a type of throat cancer. Tonsils are located at the sides of the back of the mouth. Uncontrolled growth of tonsil tissue cells causes tonsil cancer. Tonsillar squamous cell carcinoma is the most common of these cancers. Squamous cell carcinoma of the tonsil develops from thin, flat squamous cells.
The cause of tonsil cancer is unknown. Tonsil cancer can also be seen in people who have had their tonsils removed (if there is tonsil tissue left behind). Tobacco use, alcohol consumption, human papillomavirus infection, and weakened immune system are important risk factors in the development of tonsil cancer. Tonsil cancers show signs and symptoms in the early stages. Avoiding risk factors is important in tonsil cancer prevention.
The diagnosis of tonsil cancer can be made by biopsy. The effectiveness of treatment and survival rate may vary depending on the stage of cancer, the age of the patient, and the relationship of cancer to human papillomavirus (HPV) or tobacco-alcohol. The main treatments for tonsil cancers are surgery, radiotherapy, and chemotherapy. Depending on the situation, brachytherapy, targeted therapy, and immunotherapy may also be required.
Signs and Symptoms
Tonsils are one of our organs in the back of the mouth. The tonsils are located on both sides of the back of the mouth and are easily visible. Therefore, tonsil cancers, give signs and symptoms earlier than the base of tongue cancers. Tonsils are part of the immune system. Moreover, the tonsils are one of the places where the immune system first meets microbes that enter the body.
Swollen one tonsil
Having one swollen tonsil may be a sign of tonsil cancer. But, if both tonsils are swollen or enlarged, the chance of tonsil cancer is slightly lower. In addition, the normal sizes of the tonsils vary according to age and person. Normally, tonsils are larger in children. However, in adults, the size of the tonsils is slightly smaller.
Persistent sore throat
Persistent sore throat is a common symptom of tonsil cancer. Pain occurs later in tonsil cancer. This persistent throat pain hits the ear on the affected side over time, causing ear pain on one side. In terms of tonsil cancer, sore throat and ear pain on one side are serious symptoms. But, we should not confuse the sore throat of tonsil cancer with pain in the throat caused by tonsillitis and strep throat. While strep throat is more common in children, tonsil cancer is more common in elderly people and young individuals.
Lump in the neck
A lump in the neck may be the first sign of tonsil cancer. If cancer cells have spread to lymph nodes in the neck, swollen lymph nodes sign occurs. However, there are cases where tonsil cancer does not have any symptoms until its diagnosis.
Persistent sores in the throat
Especially, human papillomavirus (HPV) related tonsil cancers start in the deep recesses of the tonsils. HPV usually does not show any symptoms until it causes tonsil cancer. When it gives symptoms, it usually presents itself with sores on the tonsils, back of the tongue, and swelling in the neck. Tonsil cancer spreads to lymph nodes in the neck while it is still small and silent.
In summary, signs and symptoms of tonsil cancer may include:
Swollen tonsil on one side
Persistent throat pain
Lump in the neck
Swelling in the neck area
The feeling of something stuck in the throat
Persistent sores in the throat
Persistent tonsil infections
A red or white patch on tonsils
Difficulty in swallowing
Hoarseness
Ear pain on one side
Jaw stiffness and pain
Unexplained weight loss
Spitting up blood
Bad breath
Fatigue
Causes
The exact cause of tonsil cancer is unknown. However, several well-known factors contribute to the development of tonsil cancer. These factors are mainly tobacco use of all kinds including smoking and chewing, excess alcohol consumption, sexually transmitted human papillomavirus infections, and a weakened immune system. The role of human papillomavirus (HPV) in the formation of tonsil cancer is gradually increasing with the change of sexual behaviors. In particular, most of today’s tonsil cancers are HPV-related except for a small number.
Risk Factors
Tobacco-alcohol-related tonsil cancer is mostly the cancer of older, alcohol and tobacco user males with more comorbidities. On the contrary, HPV-related tonsil cancer is common in younger ages and both sexes. People with HPV-related tonsil cancers have less or no tobacco and alcohol use compared to the first group. However, people who do not use tobacco, do not drink alcohol, and are negative for HPV can also get tonsil cancer.
Tobacco use and alcohol consumption
It is a well-known fact that tobacco use and alcohol consumption contribute to the development of tonsil cancer. Tobacco contains many known carcinogenic substances, mainly nitrosamines, and polycyclic hydrocarbons. Alcohol turns into acetaldehyde, which adversely affects DNA repair in the cell. Especially if the amount consumed is high and these two habits are together, the risk of developing cancer increases exponentially. These are mostly the causes in elderly patients
Human papillomavirus infection
Human papillomavirus (HPV) is a sexually transmitted virus. HPV mostly causes genital cancers in women. Also, HPV can cause penile cancers in men and anal cancers. High-risk types 16 and 18 of HPV cause cancer in both the genitals and the tonsils, base of tongue, throat.
Nowadays, the role of HPV in the development of tonsil cancer has increased, especially in young people. Because especially type 16 and 18 HPV is present in many cases related to tonsil cancer. The period from the transmission of HPV to the development of cancer usually takes years. In addition, the body’s immune system can often destroy even high-risk HPV types that cause cancer. But if the immune system is weakened, the virus can cause cancer.
A weakened immune system
HPV negative elderly and young people who do not use tobacco and alcohol can also get tonsil cancer. In this respect, factors such as immunodeficiency, being an organ transplant recipient, treatments that suppress the immune system, or a weakened immune system for any reason may have an effect on the development of tonsil cancer.
In summary, factors that may increase the risk of tonsil cancer include:
All forms of tobacco use
Heavy alcohol consumption
Human papillomavirus infection
A weakened immune system
Being an organ transplant recipient
Immunosuppressive therapy
Immunodeficiency
Poor oral hygiene
Being elderly male
Environment
Genetic factors
Types of Tumors
Tonsil cancers often present as squamous cell carcinoma. However, cancers such as lymphoma, sarcoma, mucosal melanoma can also develop in the tonsils. Apart from this, there may also be metastatic cancers of the tonsils.
Squamous cell carcinoma
Squamous cell carcinoma is a type of cancer that arises from the epithelial cells lining the inner parts of the body, such as the mouth and throat. It is most common in the mouth, throat, and pharynx regions. Tonsil cancers are mostly squamous cell carcinomas. HPV-related cancers of the tonsils are also a type of squamous cell carcinoma.
Diagnosis
The patient who suspects tonsil cancer should first consult an ear, nose, and throat doctor (otolaryngologist). To diagnose tonsil cancer, the doctor first examines the patient’s mouth, throat, and neck. Later, the doctor takes tissue samples from the suspicious areas of the tonsil for examination by the pathologist. Some necessary imaging tests can also aid diagnosis.
Physical exam
After listening to the patient’s complaints, the doctor first examines the mouth, throat, and neck. In particular, the doctor looks at the tonsils and base of the tongue. In cases where the eye is missing sight, the doctor uses a special device called an endoscope. Next, the doctor checks whether the tonsil tumor has spread to the lymph nodes in the neck. For this, the doctor examines the neck and checks whether there is swelling, stiffness, or a mass.
Removing a tissue sample
The doctor takes tissue samples from the patient’s mouth, the base of the tongue, and the throat for examination by the pathologist. The doctor performs the tissue sampling from the lump in the neck with a thin biopsy needle. To avoid pain, the doctor first anesthetizes the area where tissue samples will be taken, if necessary. The doctor takes tissue samples (biopsy) in a way that does not cause excessive bleeding in the patient. A biopsy is not a procedure that will cause the tonsil tumor to spread. The diagnosis of tonsil cancer is made according to the result of the pathologist examining the tissue samples.
Imaging tests
The most common imaging tests for the head and neck region are ultrasonography (USG), computerized tomography (CT), and magnetic resonance imaging (MRI). The role of plain films and old classical X-rays in the diagnosis of head and neck cancers has decreased. Positron emission tomography (PET) is an important imaging test to investigate the spread of the tonsil tumor to distant regions.
Treatment
Treatment of tonsil cancer may vary depending on the type of cancer, its relationship with HPV, its stage, and the patient’s general health and preference. Surgery is often the first treatment for tobacco-alcohol-related tonsil cancers. Chemoradiation is more effective and more prominent today in HPV-associated tonsil cancers that are more common. Chemoradiation is a combined therapy consisting of radiation therapy and chemotherapy.
With the combined use of radiation therapy and chemotherapy, the success rate of HPV-associated tonsillar squamous cell carcinoma treatment has increased considerably. On the other hand, chemoradiation is the first choice in these situations as it affects swallowing and speech, less than surgery. However, in general, surgery is an effective treatment for many stages of tonsil cancer. Brachytherapy, targeted therapy, and immunotherapy may also be necessary for the treatment of tonsil cancers.
Treating doctors
Mainly otolaryngologists – head and neck surgeons take over the diagnosis, treatment, and surgery of tonsil cancer. Radiation oncologists participate in treatment for radiation therapy and medical oncologists for chemotherapy. Depending on the situation, plastic surgeons, dentists, speaking, nutrition, swallowing, and pain management specialists also take part in the treatment process.
Surgery
Surgery is generally at the forefront in the treatment of tobacco-alcohol-related cancers of the tonsils. Because surgery has much applicability and therefore its effectiveness is more. TransOral Robotic Surgery (TORS) can be advantageous in areas that are relatively difficult to reach orally. These areas are the back of the mouth and the base of the tongue. Removing some tonsil tumors requires extensive surgery. Radiation therapy and chemotherapy are added to the surgical treatment of HPV-negative tonsil cancers according to the stage of cancer.
Tumor removal
The surgeon decides how to remove the tonsil tumor. And the surgeon also decides how much of the surrounding area will be removed based on a preoperative examination, biopsy, and imaging tests. The head and neck surgeon often removes the tonsil tumor by entering the mouth. However, depending on the size of the tumor and its spread to the surrounding tissues, it is possible to remove the tumor by incision from the neck. The surgeon removes the tonsil tumor with some border of healthy tissue around it. The surgeon performs this procedure to ensure that no cancerous tissue is left behind.
Lymph node removal
Tonsil cancers can spread to lymph nodes in the neck. Therefore, it is necessary to remove the lymph nodes in the neck during surgery. Lymph nodes, which are likely to contain metastases, are removed from the neck for precautionary purposes. Because cancer cells hidden in them can cause other head and neck cancers in the future. The surgeon usually removes the cancerous tissue and lymph nodes in the neck in the same surgical session.
Reconstruction
After removing the tonsil tumor, the surgeon takes tissue samples from the surrounding healthy tissue borders. The pathologist examines these tissue samples in the pathology laboratory. After the pathologist reports the tissue samples as clean, the surgeon moves to the stage of repairing the surgical wound.
After removing the cancerous tissue, the surgeon tries to repair the cavities by closing them with surrounding tissues (reconstruction). If the tissue is not sufficient to close the surgical space, the surgeon can take tissue from the more distant areas of the body. These areas are the anterior chest wall, forearm, hip, leg, etc.
Normalization process after surgery
After surgery, the patient can stay in the hospital for a while. Depending on the size of the surgery, the patient may spend a few days in the intensive care unit. In the first days after surgery, the patient has a urinary catheter, some tubes, and probes to drain the blood and fluid accumulation from the surgical wound. These are removed gradually over the next few days as the patient recovers.
The patient also takes intravenous painkillers and antibiotics to relieve pain and prevent possible infections. If the patient has other health problems such as diabetes, heart disease, blood pressure, it will be necessary to keep them under control with drugs. After a while, surgical wounds in the patient’s mouth and throat heal. The patient starts feeding with liquid and soft foods orally. After the patient can eat normally and speak easily, the hospitalization period ends.
Radiation therapy
In cases where tonsil cancer has not completely disappeared by surgery or there is a possibility that cancer has spread to the lymph nodes, the patient receives post-surgical radiation therapy. But first, the patient should recover after tonsil surgery. A radiation oncologist delivers radiation therapy to the patient with a radiation-emitting device. Radiation therapy uses high-powered energy beams to kill cancer cells.
If tonsil cancer has not spread to surrounding tissues, radiation therapy may be sufficient alone as the first treatment. In particular, HPV-related tonsil cancer responds very well to radiation therapy. Radiation therapy is used in combination with chemotherapy (chemoradiation) as an alternative to surgery. In particular, in cases where surgery is not possible for various reasons, the patient receives radiation therapy for cancer regression. Radiation therapy is also useful in preventing the recurrence of tonsil cancer. But generally, radiation therapy is an additional post-surgical treatment.
Brachytherapy
If tonsil cancer is still present after the main treatments (surgery, radiation therapy, and chemotherapy) are completed, the radiation oncologist delivers brachytherapy. Brachytherapy is a different type of radiation therapy. In brachytherapy, the radiation oncologist places small tubes containing radioactive material around the tonsil tumor for a certain period of time for treatment. These tubes emit radioactive rays that particularly affect cancer cells.
Chemotherapy
Medical oncologists administer chemotherapy. The goal of chemotherapy is to destroy cancer cells using powerful anti-cancer drugs. Chemotherapy drugs reach cancer cells through the bloodstream. Also, chemotherapy makes cancer cells more vulnerable to radiation and increases the effectiveness of radiation therapy. In this respect, chemotherapy is often added to radiation therapy. In particular, chemotherapy is a routine part of treatment for HPV-related tonsil cancers that respond well to radiation therapy.
Targeted therapy
Targeted therapy is a treatment using drugs that cause little damage to healthy cells and target mainly cancer cells. The effect of these drugs is different from traditional chemotherapy drugs. In particular, the side effects of targeted therapy drugs are generally milder than chemotherapy drugs. In the treatment of tonsillar cancer, targeted therapy is often combined with chemotherapy. Medical oncologists also undertake targeted therapy.
Immunotherapy
They are medical oncologists who administer immunotherapy. Immunotherapy plays an important role mainly when cancer has progressed and other treatments are not an option. Cancer cells produce proteins so that immune system cells don’t notice them. In this case, the immune system cannot attack cancer cells. Therefore, immunotherapy strengthens the immune system, making it more resistant and more effective against cancer.
Speech functions after surgery
Surgeries in the tonsil area can affect speech function. But, after the surgical wounds in the mouth and throat of the patient heal, his speech becomes clearer. The pronunciation of some letters and words may be less clear after surgery. However, this rarely becomes a communication problem for the patient. In these situations, speech therapists can assist the patient. In addition, there are also successful surgical procedures aimed at solving speech problems that may develop after tonsil cancer surgery.
Taste functions after cancer treatment
After tonsil cancer surgery, there is usually no deterioration in taste. First of all, the patient can’t taste in the first postoperative days. Because during this period, the patients cannot feed orally anyway. However, if the patient has also received radiation therapy, there may be taste disturbances for a while. Radiation therapy, due to its side effects, can lead to decreased saliva secretion and dry mouth. In these cases, ADA approved mouth moisturizers (eg, Biotene Dry Mouth Oral Rinse, or as a different choice: TheraBreath Dry Mouth Oral Rinse, etc.) may be beneficial for the patient.
Feeding after surgery
Depending on the size of the tonsil cancer surgery, surgical wound repair, and additional post-surgical treatments, the patient cannot feed orally for a while afterward. Instead, the patient feeds with special nutritional fluids through a tube extending from the nose to the stomach or intravenously. After the surgical wounds in the patient’s mouth and throat heal, the patient begins to feed orally with liquid and soft foods. Over time, the patient can easily feed and swallow. Some successful surgical procedures will alleviate or eliminate swallowing problems that may develop in the patient after tonsil cancer surgery.
Prognosis
The survival rate in tonsil cancers depends on the type of tumor, its relationship with human papillomavirus (HPV), its stage, and how far it has spread. In particular, HPV-related tonsil cancer in young patients responds better to current treatments. HPV-negative tonsil cancers in older patients, on the other hand, have a relatively poor prognosis.
Treatment of tonsil cancer is often possible. Especially, the success rate of treatment in the early stage of tonsil cancer is high. However, there are many things the doctor can do in the late stages of tonsil cancer or in case of delayed treatment.
Follow-up care
In patients who have received treatment for tonsil cancer, the probability of recurrence of the cancer is higher in the first years. Therefore, the patient comes to the doctor’s control at certain intervals for a while after the treatment process. If the patient complies with these controls, the follow-up period usually takes up to 5 years. Recurrence of tonsil cancer after the fifth year is not considered as coming back. The doctor considers this condition new cancer.
Recurrence of cancer after treatment
Recurrence of tonsil cancer does not mean that the patient has no chance. Because additional surgery is still possible if the patient has only previously undergone radiation therapy and chemotherapy. Especially, surgery is still possible if the cancerous tissue can be removed completely. If repeat surgery will not be possible in the patient, an additional dose of radiation therapy comes into prominence.
The reality is that effective radiation therapy to a particular area is usually only possible once. However, when necessary, the radiation oncologist may deliver radiation therapy at a lower dose to the same area. In such cases, brachytherapy is another option. For chemotherapy, a situation like radiation therapy is not valid. But, the patient can receive chemotherapy treatment repeatedly as long as his body, organs, and immune system allow.
Tonsil Cancer Prevention
Don’t use tobacco products
To reduce the risk of developing tonsil cancer, it is necessary to avoid tobacco use. Especially, the patient treated for tonsil cancer should definitely stop any tobacco use, including smoking and chewing, to minimize the chance of cancer recurrence. If the patient cannot quit smoking, a psychiatrist or psychologist will help.
Stop or limit alcohol use
To reduce the risk of developing tonsil cancer or recurrence of tonsil cancer, it is necessary to quit alcohol, if any. If it is difficult to quit alcohol, it is necessary to try to limit its use. Even the use of alcohol-containing oral care products is risky in terms of regularly and repeatedly exposing the mouth to alcohol. In this respect, the use of alcohol-free products (eg, ADA approved mouthwash: TheraBreath Fresh Breath, CloSYS Sensitive Gentle Mint, CloSYS Ultra Sensitive Unflavored, or as a different choice: Tom’s of Maine Natural Wicked Fresh, etc.) is very important.
Protect yourself against HPV
It is important to prevent HPV infection because of its increasing role in the development of tonsil cancer. Therefore, safe sex is very important in this regard. However, condoms alone will not protect the person from HPV. Because HPV infection can also occur during oral sex. A full course of HPV vaccine may also be helpful to reduce the risk of HPV transmission.
Get regular dental checkups
Many tonsil cancers are first detected during regular dental checkups. Therefore, regular dental checkups are important for the early detection of tonsil cancer. Dentists can also detect precancerous lesions of the mouth at earlier stages.
Live a healthy life
HPV-negative people who do not use tobacco and do not consume alcohol can also get tonsil cancer. Therefore, it will be beneficial to exercise regularly, eat a healthy diet, give importance to oral hygiene to reduce the risk of developing tonsil cancer. In addition, keeping immunity and morale high is also important.
References
American Cancer Society: “Can oral cavity and oropharyngeal cancers be prevented?”
American Cancer Society: “Surgery for Oral Cavity and Oropharyngeal Cancer”
Mayo Clinic: Diseases and Conditions, “Tonsil Cancer”
National Center for Biotechnology Information (NCBI): “Tonsil Cancer”
NCCN Clinical Practice Guidelines in Oncology: “Head and Neck Cancers, Version 2.2020”
Penn Medicine, Throat (Oropharyngeal) Cancer, “Types of Throat (Oropharyngeal) Cancer”