Parotid Gland Cancer
The parotid is the largest salivary gland and salivary gland tumors most frequently develop from here. Parotid gland tumors include benign and malignant tumors (parotid gland cancer). Most parotid tumors are benign, and pleomorphic adenoma of the parotid gland is the most common. Warthin’s tumor is the second most common benign parotid tumor. The most common parotid cancer is mucoepidermoid carcinoma, followed by adenoid cystic carcinoma and adenocarcinoma of the parotid gland.
Tumors mostly develop from the superficial lobe of the parotid and show early signs and symptoms compared to deep lobe parotid tumors. The reasons for the occurrence of parotid gland tumors are not clear. Risk factors such as tobacco use, exposure to radiation including mobile phones, exposure to chemicals, and alcohol consumption may have an impact on the development of parotid gland cancer. Avoiding risk factors may be beneficial in parotid cancer prevention.
The diagnosis of a parotid gland tumor can be made by biopsy. The survival rate may vary depending on the type of parotid gland cancer, its spread, the age, and the general health status of the patient. Normally, the main treatment for a parotid gland tumor is surgery. When necessary, radiation therapy and sometimes chemotherapy take part in the treatment of parotid gland cancer.
The Parotid Gland
There are 3 pairs of major salivary glands. These are the parotid, submandibular and sublingual glands. Apart from these, there are also many minor salivary glands. The parotid is the largest salivary gland, although it makes less saliva than the smaller submandibular gland.
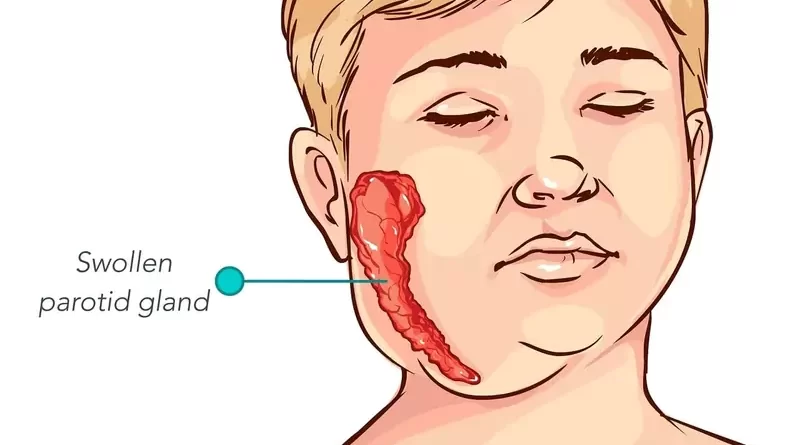
On the face, the parotid extends from the front of the ear lobule down to the jaw corner. The saliva-carrying parotid duct (Stensen’s duct) opens into the mouth, to the right-left inner cheeks at the level of the upper second molar teeth.
Our facial nerve that provides facial movements passes through the right and left parotids. The facial nerve branches off inside the parotid gland that will go to the facial muscles.
The part of the parotid gland under the facial skin and above the facial nerve is its superficial lobe. And the other part of the parotid gland under the facial nerve and in the posterior-deep part of the jawbone is its deep lobe. Most parotid gland tumors develop from the superficial lobe of the parotid gland. Tumor rarely develops from the deep lobe.
Of all salivary glands, tumors most commonly develop from the parotid gland. In general, as the size of the salivary gland increases, the risk of malignancy of the tumor decreases. Most parotid tumors are benign, as the parotid is the largest salivary gland.
Signs and Symptoms
A typical benign parotid gland tumor is a tumor that the patient has noticed for a long time and grows very slowly (over months and years) during this time. However, if the patient delays treatment, the benign tumor may turn into a parotid cancer over time. Parotid cancer, although there are exceptions, is a tumor that develops in a shorter time and grows rapidly (within weeks or months).
Salivary stones (sialolithiasis) obstructing the parotid duct are less common than its tumors. However, sialolithiasis is a common disease of the salivary glands and occurs mostly in the submandibular gland and less frequently in the parotid gland. This situation can lead to swelling, redness, and pain that occurs occasionally and then heals in the parotid. These stones can sometimes cause inflammation of the salivary gland (sialadenitis).
In case of inflammation of the parotid, swelling, pain, and redness of the gland increase. Improvement occurs with antibiotic treatment or stone dislocation over time. However, the swelling due to the parotid tumor does not regress, on the contrary, it continues to grow.
Lump in the cheek on one side
The parotid tumor manifests as swelling, lump, mass, or growth in front of or below the ear lobule on one side, which has usually been present for more than 2-3 weeks. Although parotid gland tumors are sometimes two-sided (eg, Warthin’s tumor), they are mostly one-sided.
Benign parotid gland tumors are firm and rubbery. The mass moves easily when held between two fingers. However, malignant tumors are harder and are fixed to the overlying skin, underlying tissue (muscle, bone). Therefore, they are relatively difficult to move between the fingers. Even benign parotid gland tumors are usually firm, but a rock-hard mass generally denotes malignancy.
Subsequent facial pain on one side
Whether parotid gland tumors are benign or malignant, they are usually painless. However, as parotid gland tumors develop, as they invade or compress surrounding tissues (for example, the facial nerve), pain occurs. In this respect, especially, a parotid gland cancer can manifest itself with persistent pain that starts later. If there is pain, it most likely indicates perineural invasion or association with the mass.
Paralysis of one side of the face
The parotid cancer that invades the facial nerve passing through the parotid gland may cause numbness, tingling, weakness, and paralysis of the facial muscles on that side. Facial nerve weakness or paralysis rarely accompanies benign lesions and indicates mostly malignancy.
Swollen lymph nodes in the neck on one side
Since benign parotid gland tumors do not spread to the neck lymph nodes, they do not cause swelling in the neck. However, malignant tumors have the potential to spread to lymph nodes in the neck. In this case, they cause neck swelling. In general, many patients with facial nerve paralysis have neck lymph node metastasis.
Tethering or ulceration of overlying skin
If parotid gland cancer is close to the skin, it may cause changes, redness, or ulcers of overlying skin. Benign tumors do not cause such changes in the skin.
No symptoms
Since deep lobe parotid tumors are behind the jawbone, they are detected later than superficial lobe tumors. Because the tumor is in the deep parts of the neck, the patient does not have any noticeable swelling. Head and neck imaging tests taken for other reasons sometimes detect deep lobe parotid tumors incidentally.
Causes
There are serious doubts that factors such as tobacco use, exposure to radiation including mobile phones, occupational exposures to chemicals, and alcohol consumption can cause parotid cancer. But there is no clear evidence yet. Viruses, diet, or other factors have also not been proven to cause parotid cancers. The causes of benign parotid tumors are much more uncertain.
Risk Factors
Parotid gland tumors develop usually in the middle and older ages. But it can develop at any age, including childhood. However, benign parotid tumors are more common in the young and middle age group, while malignant tumors are more common in the older age group. Apart from that, malignant parotid gland tumors in children and young adults are relatively slow-growing tumors with low malignancy potential. These malignant tumors follow a similar course to benign tumors.
The incidence of parotid gland tumors is equal between men and women. However, Warthin’s tumor, which is a benign parotid tumor, is more common in men.
Being older
Although parotid gland tumors can occur at any age, parotid cancers are most common in older adults, most frequently in the sixth decade.
Tobacco use
Warthin’s tumor, which is a benign parotid tumor that is more common in men, is associated with tobacco use. Because this tumor is more common, especially in tobacco users. Apart from this, tobacco use is also a risk factor in the transformation of benign parotid tumors into parotid cancer.
Exposure to radiation
Exposure to radiation (for example, radiation therapy) is a risk factor for parotid cancer. Apart from this, today’s mobile phones also affect the parotid gland at close range. In this respect, some doubts focus on the electromagnetic effect emitted by the mobile phone.
Exposure to chemicals
Regular occupational exposures may increase the risk of parotid cancer. The chemical industry, mining, sanitary work, rubber or nickel industries are among the risky areas in terms of parotid gland tumors.
Alcohol consumption
Unlike other head and neck tumors associated with alcohol consumption, the role of alcohol in salivary gland tumors is unclear. The relationship between alcohol consumption and parotid cancer has not yet been confirmed.
Types of Parotid Tumors
A tumor refers to the mass of uncontrolled proliferating cells. There may be a tumor of any tissue in the body. There are also tumors of the salivary glands. Tumors are generally benign or malignant. Tumors of the parotid gland can also be benign or malignant. Most parotid gland tumors are benign tumors. We call the malignant tumor of the parotid gland simply parotid cancer.
Benign parotid tumors
Benign parotid gland tumors grow slowly. This growth occurs over months, even years. A thin, membranous sheath (capsule) usually surrounds benign parotid tumors. Benign parotid tumors do not invade surrounding tissues. They usually grow by pushing the surrounding tissues and making room for themselves. Benign parotid tumors do not metastasize to neck lymph nodes and distant parts of the body. The most common benign parotid gland tumors are;
Pleomorphic adenoma (benign mixed tumor)
Pleomorphic adenoma is the most common salivary gland tumor and is most common in the parotid. The pleomorphic adenoma of the parotid gland, which is a benign tumor, is more than half of parotid gland tumors. These tumors are slow-growing and cause no symptoms. Pleomorphic adenoma is the second most common benign parotid gland tumor after hemangiomas in childhood.
Although pleomorphic adenomas are benign, they tend to recur. Apart from that, if they are not completely removed, there is a risk of turning into a malignant tumor over the years. In this case, the mass that has been growing slowly for years begins to grow rapidly. One-tenth of pleomorphic adenomas that have existed for more than 15 years can become cancerous.
Warthin’s tumor
Warthin’s tumor, also known as papillary cystadenoma lymphomatosum, is the second most common benign parotid tumor. These tumors almost always develop from the parotid gland, with a tenth of them found in both parotid glands. Warthin’s tumor is in the form of a soft mass.
Basal cell adenoma
Basal cell adenoma is a benign tumor that mostly develops from the parotid gland but we can also see it in other salivary glands.
Oncocytoma
Oncocytoma develops mostly from the parotid gland and is a benign tumor. However, it can also develop from other salivary glands. Oncocytoma originates from a type of salivary gland cell called oncocyte.
Other benign parotid tumors
Benign tumors such as canalicular adenoma, myoepithelioma, and sialoadenoma papilliferum, which are less common, may also develop from the parotid gland. Apart from this, masses originating from vessels such as hemangioma, lymphangioma (cystic hygroma) and salivary gland cysts may also occur in the parotid.
Parotid Cancer
Malignant tumors of the parotid are less common than benign tumors. These tumors grow rapidly (within weeks and months) with some exceptions. They can metastasize to neck lymph nodes, lungs, liver, brain, bone, and other distant areas. Parotid gland cancers are usually not encapsulated. They invade surrounding tissues (eg facial nerve) and develop by disrupting their functions.
Some tumors develop from the blood vessels and lymph nodes in the parotid gland. Even malignant tumors (eg squamous cell carcinomas) that occur in areas such as the scalp, cheeks, nose, eyelids but spread to the lymph nodes in the parotid may also be. The most common malignant parotid tumors are the following;
Mucoepidermoid carcinoma
Mucoepidermoid carcinoma is the most common malignant tumor of the salivary glands as well as the parotid gland. Relatively slow-growing types are common, but there are also fast-growing types. The patients are generally middle-aged and older adults, but there may be younger patients.
Adenoid cystic carcinoma
Adenoid cystic carcinoma is another of the most common parotid gland cancer. A well-known feature of this tumor is that it penetrates the nerve fibers in its area and uses them as a way to spread. Adenoid cystic carcinoma may show little change over a long period of time and then suddenly spreads extensively to surrounding tissues.
Adenoid cystic carcinomas spread through the blood rather than lymph. Metastases of adenoid cystic carcinomas to the lungs are quite common. They tend to recur, sometimes years after surgery and radiation therapy. Adenoid cystic carcinomas are more common in people of middle age and older.
Acinic cell carcinoma
Acinic cell carcinoma is a type of adenocarcinoma. It is a tumor with low malignancy potential and grows slowly. Although it is malignant, it is encapsulated tumor and less likely to spread to distant sites. Acinic cell carcinoma accounts for about one-tenth of malignant salivary gland tumors. Nine-tenths of acinic cell carcinomas develop from the parotid.
Acinic cell carcinoma may develop in children and elderly people. Acinic cell carcinoma, which is mostly a tumor of young adults, has a better prognosis compared to other parotid gland cancers. It can occur in both parotid glands at the same time. This tumor also may spread along nerve fibers.
Malignant mixed tumors
The malignant mixed tumor is one of the malignant tumors of the parotid gland specific to elderly people. Carcinoma ex pleomorphic adenoma is the most common type of these tumors. It is the untreated form of pleomorphic adenoma that has turned into a malignant tumor over many years. In this case, the mass of the parotid that has existed for years suddenly begins to grow rapidly. Carcinoma ex pleomorphic adenoma is a highly aggressive tumor with very low cure rates.
Adenocarcinoma
Many types of adenocarcinomas can be seen in the parotid gland. Some of these tend to have low malignancy potential (eg, acinic cell carcinoma, polymorphous adenocarcinoma). But types such as oncocytic carcinoma and salivary duct carcinoma are more likely to have high malignancy potential and have less positive outcomes.
Other cancers
Cancers such as squamous cell carcinoma and Non-Hodkin lymphoma are also sometimes seen in the parotid gland. Squamous cell carcinoma occurs mainly in older people. It may develop after radiation therapy in the area and tends to have a poorer outlook.
Non-Hodgkin lymphoma can rarely start from immune system cells in the salivary glands. The risk of lymphoma is increased in patients with Sjögren syndrome. Non-Hodgkin lymphomas may develop in both parotid glands at the same time. Lymphoma occurs most commonly in elderly people.
Metastasis from other sites
The parotid also may be the site of metastasis from skin, lung, breast, prostate, renal, or gastrointestinal tract malignancies.
Diagnosis
A patient who suspects parotid salivary gland cancer should first consult an ear, nose, and throat doctor (otolaryngologist). The diagnosis process begins when the patient notices a swelling and mass in front of or below the ear lobule and consults a doctor. The doctor first listens carefully to the patient’s complaints. History is important in distinguishing inflammatory from tumoral masses. The doctor asks the patient various questions about the symptoms and asks whether the patient’s history and family have experienced such situations. Then the examination phase starts.
Physical exam
The otolaryngologist usually performs a thorough examination of the ear, nose, mouth, throat, and neck, regardless of the reason the patient applies to him. The doctor examines the entire head and neck for cutaneous lesions, which may represent malignancies that could metastasize to the parotid gland. Then, the doctor carefully examines the mass in terms of size, stiffness, mobility, adhesion to surrounding tissues. Next, the doctor checks for reduced movement or weakness in the facial muscles.
Imaging tests
If the parotid gland tumor does not have a relationship with the oral cavity or throat, imaging tests are performed before tissue sampling. These imaging tests are ultrasonography (USG), magnetic resonance imaging (MRI), or computed tomography (CT).
Ultrasonography is often the first imaging test the physician applies because it is the easiest to access. It is the preferred tool for the initial assessment of tumors in the superficial parotid. Ultrasound imaging of superficial structures of parotid is excellent and it does not carry any risk of radiation. The radiologist evaluates the image of the mass on ultrasonography.
Magnetic resonance imaging provides much more information about soft tissues and their properties compared to computed tomography. But, CT scanning provides better detail of the surrounding tissues. In particular, it is important to visualize large or deep parotid lobe tumors, preferably by MRI.
The radiologist can also perform magnetic resonance imaging by administering intravenous drugs (contrast material). This method has become an important imaging test to examine the parotid gland tumor.
In parotid gland tumors that may have spread to distant organs, imaging tests such as positron emission tomography (PET) and computer tomography (CT) may be required.
Removing a tissue sample
If the tumor is associated with the mouth or throat, the doctor takes tissue samples by making an incision. But if the tumor has developed as a lump under the skin and the mass does not have any relation to the oral cavity or throat, a needle biopsy is a safe method to take tissue samples.
Taking tissue samples from the mass by cutting the skin can damage the facial nerve. Apart from this, it may cause the tumor to spread and treatment may be more difficult. In this respect, a biopsy is not taken from the mass with a skin incision unless the tumor reaches the skin.
During a needle biopsy, the doctor often uses ultrasound to guide the needle. Needle biopsy is a procedure that does not cause much physical discomfort and pain to the patient. After the biopsy procedure, the patient can often return to his daily life.
The pathologist examines and interprets the cell and tissue samples taken from the parotid, then reports to the surgeon. However, the surgeon sometimes skips the preoperative biopsy stage and surgically removes the entire tumor. Then, the pathologist examines the tumor in detail and makes a diagnosis.
The biopsy may not always lead to an accurate diagnosis. However, a detailed examination of the completely removed mass by the pathologist leads to a more definite diagnosis. In this respect, the diagnosis made by biopsy in salivary gland tumors may change in post-surgical pathological examinations.
Treatment
Any tumor of the parotid, whether benign or malignant, needs to be surgically removed. Because the benign tumor of the parotid continues to grow, albeit slowly, and surgery becomes difficult. Apart from this, there is a risk that the benign parotid tumor may turn into a parotid cancer over time. Moreover, there are parotid gland tumors of unknown nature, between benign and malignant tumors
In the treatment of parotid tumors, after surgery, the patient receives radiation therapy and sometimes chemotherapy when necessary. However, if the patient has serious health problems that do not allow surgery, or if the parotid gland tumor has spread so that its complete removal is not possible, other treatment options without surgery may become important.
Treating doctors
Problems with the parotid gland are among the areas of interest of otolaryngologists. Otolaryngologists, experienced in head and neck surgery perform the surgical treatment of parotid tumors. Radiologists, neurosurgeons, plastic surgeons, radiation oncologists, medical oncologists, and psychologists can also participate in the diagnosis and treatment of parotid tumors. In case of suspicion of a parotid gland tumor, it is necessary to consult an experienced otolaryngologist first.
Surgery
The surgeon performs parotid tumor surgery under general anesthesia with an incision extending from the front of the ear lobule to the neck. However, depending on the location of the tumor in the salivary gland, the surgeon may also perform parotid tumor surgery via an intraoral approach.
Finding the facial nerve during surgery and preserving it with all its branches as much as possible is as important as removing the tumor. The nerve monitor device makes it easy for the surgeon to recognize and protect the facial nerve during surgery.
Botox, which is a very common cosmetic application today, makes it difficult for the nerve monitor device to work. The effect of botox on facial muscles can last up to six months. In a facial surgery performed during this period, the nerve monitor may be dysfunctional. If the patient has had botox in the last 6 months, the surgeon should definitely know this.
Tumor removal
To reach the parotid gland tumor, the surgeon makes an incision that starts just in front of the ear, passes below the ear, turns back, and then extends to the neck. In order not to notice the incision, the surgeon usually makes it through the skin folds. The protection of the facial nerve that passes through the parotid and branches off is the most critical stage during tumor removal.
The surgeon usually removes the superficial lobe of the parotid above the facial nerve together with the tumor (superficial parotidectomy). To remove the deep lobe parotid tumors under the facial nerve, the surgeon first removes the superficial lobe of the gland. Then the surgeon exposes the facial nerve and its branches and removes the deep tumor without damaging them. At this time, the surgeon removes the entire parotid gland (total parotidectomy). However, it is normal for some healthy salivary gland tissue to remain, despite being named as total.
If the parotid tumor is benign, the surgeon can perform all these procedures relatively easily. Surgery becomes relatively difficult if parotid gland cancer involves the facial nerve, or invades it.
Lymph node removal
Parotid gland cancer can spread to the neck lymph nodes. In this case, during the removal of the tumor, the surgeon removes the suspicious lymph nodes on the same side with the highest probability of the tumor spreading (neck dissection) with the incision made in the neck. Neck dissection is required especially for parotid gland tumors with intermediate and high malignancy potential. Neck dissection may not be required for tumors with low malignancy potential.
There is no place for neck dissection in benign parotid gland tumors. However, sometimes the surgeon performs neck dissection with a second surgery for tumors that are malignant in post-surgical pathological examinations.
Neck dissection is a standard treatment for malignant tumors located in the face, head, and neck regions. It is often a separate surgery that the surgeon performs during tumor surgery. Neck dissection has a therapeutic purpose in case of metastasis of the tumor to the neck lymph nodes. However, the surgeon can also do it as a precaution against future metastases even when there is no visible metastasis.
Reconstruction
After removing the parotid tumor, the surgeon goes into the repair phase. During surgery, the surgeon can remove skin, muscle, bone, or nerve tissue along with the tumor. In this case, the surgeon may require skin, muscle, bone, or nerve transfers from other parts of the patient’s body to restore cosmetic and functional repair of the face, jaw, or neck.
Normalization after surgery
After parotid tumor surgery, the patient usually stays in the hospital for a few days. The patient carries the tube placed to expel blood and fluid from the surgical wound for one or two days. A tight bandage remains for a few more days to prevent blood and fluid accumulation at the surgical site.
After surgery, the pain is rarely difficult to bear. In the first few days, pain relievers are sufficient to relieve this pain. The doctor gives antibiotics to the patient for a few days in case of infection.
As a result of blood and fluid accumulation, there may be swelling in the face and neck areas for a few days after surgery, but these will pass over time. Apart from this, there may be pain due to bandages and swelling in the forehead and ear after surgery. These will pass after the patient has relieved the bandage.
Radiation therapy
The radiation oncologist gives radiation to the parotid tumor area and the regions where the tumor is likely to spread, with special devices. After surgery for parotid cancer with intermediate or high malignancy potential, the patient receives radiation therapy after recovery from surgery. Very rarely, some persistent benign tumors may also require radiation therapy. But, the use of radiation therapy in these cases is controversial and is sometimes not recommended. Because especially in younger patients there is a risk for radiation-induced tumors.
Radiation therapy is applied to increase the effect of surgical treatment of parotid cancers. Radiation therapy increases the patient’s chance of getting rid of parotid cancer. However, radiation therapy cannot be the sole primary treatment for parotid cancers.
Chemotherapy
Chemotherapy uses anti-cancer drugs which kill cancer cells in the body. Medical oncologists deliver chemotherapy. Chemotherapy generally has no place in the standard treatment of salivary gland tumors, including parotid tumors. Even parotid gland cancer responds poorly to chemotherapy.
The usage of chemotherapy is highly common in the treatment of lymphoma of the salivary gland. Apart from this, the doctor may add chemotherapy in the presence of metastases and in the treatment of parotid cancers that cannot be completely removed or recurred. Treatment of parotid tumors with medication alone will not work unless there is an inflammation-like condition. No chemotherapy has been proven effective as the sole treatment.
Targeted therapy
It is still unclear whether targeted therapy drugs are effective in the treatment of parotid cancers. Targeted therapy research is still at an early stage in the treatment of parotid cancers.
Facial nerve functions after surgery
A parotid tumor may cause weakness and asymmetry in facial mimics, especially when smiling, by affecting the facial nerve on the side it is located. In cases that the tumor affects the facial nerve too much, weakness occurs in the forehead, eyelid, rim, and nose wing muscles. If the tumor affects the facial nerve, the weakness in the facial muscles of the patient passes within weeks after surgery.
If the parotid tumor has surrounded or infiltrated the facial nerve, the surgeon can remove the facial nerve during surgery. In such cases, the patient already has a certain degree of facial weakness and paralysis before surgery.
In cases where the facial nerve is removed due to a tumor, the surgeon repairs this nerve with a nerve graft taken from another part of the body. The greater auricular nerve as a donor is an option. But, the sural nerve from the leg may be also preferred. But even inexperienced hands, the facial nerve rarely fully heals functionally.
Salivary functions after surgery
There are three pairs of major and many minor salivary glands opening into the mouth with various ducts. The surgeon may remove one of these salivary glands due to the tumor. However, this does not lead to a reduction in the amount of saliva, dry mouth, or impairment of digestive functions. The remaining major and minor salivary glands take over the function of the missing gland. However, if the patient has received radiation therapy after surgery, the patient may experience decreased saliva and dry mouth for a while. In these cases, ADA approved oral rinse (eg, Biotene Dry Mouth Oral Rinse, or as a different choice: TheraBreath Dry Mouth Oral Rinse, etc.) may be beneficial for the patient.
Frey syndrome after surgery
Frey syndrome is a problem that can occur months after parotid gland surgery. This situation presents itself in the form of sweating and redness on the surgically treated side of the face during meals. The reason for this is that the nerves that go to the salivary gland and activate saliva production reach the sweat glands in the skin after surgery. This rare occurrence is often tolerable by the patient.
Appearance and face symmetry after surgery
The surgeon performs parotid tumor surgery with an incision created under aesthetic principles, extending from the front of the ear lobule to the neck. The scar of this incision may be slightly evident while healing after surgery. This situation, which is more common in dark-skinned people, is mostly related to the genetic characteristics of the person. But this problem is very rare.
To prevent the surgical incision from healing with a distinct scar, patients should not show the incision area to the sun for up to a year. The patient should protect the incision area with high protection factor creams or clothing accessories when outdoors. In addition, some cream or gel-form medications can make the surgical incision scar less obvious
After surgeries performed due to large tumors of the parotid, a dimple may occur in front of or below the ear. With the increase of adipose tissue over time, this area is likely to be filled spontaneously. Generally, the patient does not feel much about the lack of healthy salivary gland tissue removed along with the tumor.
Speaking and feeding after surgery
After surgery, the patient is not given food or liquid orally for a few hours until the effect of anesthesia disappears. Later, the patient starts to feed with soft, liquid foods, and gradually switches to normal foods.
After extensive tumor surgeries, it may take longer for the patient to recover and switch to the old diet. However, functions such as nutrition and speaking are not permanently affected unless there are interventions such as removal of the nerve, muscle, jawbone, or neck skin due to parotid cancer.
The secretion formed by the salivary glands not only helps digestion but also provides the necessary wetness and moisture for the mouth and throat cavities. In addition, saliva creates a defense mechanism against microorganisms that cause infection. Therefore, the side effect of radiation therapy that causes a decrease in saliva secretion may cause sores on the skin, mouth, and throat after a while. After these heal over time, the patient’s salivation and swallowing problems also disappear.
Prognosis
The prognosis for parotid cancers is better in children and adolescents. The main reasons for this are low frequency of metastasis, low spread, and tumors with low malignancy potential. Overall survival for children after surgical treatment is better than for adults.
The survival rate in parotid cancer mostly depends on the type, stage, size of cancer, distant metastasis, older age, and comorbidities. In parotid cancers, distant metastases most commonly occur to the lungs, bone, liver, and brain. Distant metastases are one of the main causes of death. So, if parotid cancer is found early and treated, the prognosis is good.
Follow-up care
Regular medical check-ups after parotid cancer treatment aim to detect recurrence and manage any treatment complications that may occur. Long-term follow-up is very important for parotid cancers. Most recurrences occur in the first 3 years after treatment. Patients should receive regular follow-up at regular intervals within 5 years after treatment. Then, regular follow-up should continue every 1 year.
Parotid gland tumors require surveillance for up to 20 years after treatment. In particular, extra care should be taken for adenoid cystic carcinoma due to delayed recurrence or propensity for metastasis. Due to the high risk of lung metastases, annual breast screening should be performed for tumors with high malignancy potential. Patients who receive neck radiation should have their thyroid hormone levels checked several times a year.
Recurrence of parotid cancer
Approximately half of the malignant salivary gland tumors recur after initial treatment. Parotid gland tumors can recur after treatment. In these cases, if possible, the surgeon attempts to remove the tumor completely by surgery. Repeat surgeries are more difficult after cancer recurrence. Because facial nerve recognition and protection will become more difficult due to the healed tissues caused by the previous parotid surgery. The importance of the nerve monitor device is more in repeat surgeries after cancer recurrence.
Prevention
There is little information about the causes of parotid cancers. Information on the causes of benign parotid tumors is more limited. In this respect, ways to prevent parotid tumors are also unclear. However, it is thought that avoiding certain things may be beneficial in preventing parotid cancer.
Quit smoking
Some parotid gland tumors are more likely to be associated with tobacco use (eg, Warthin tumor). Especially if the person is older, this risk will increase even more. One can reduce the risk of developing parotid cancer by avoiding tobacco use, which is associated with many head and neck cancers.
Reduce radiation exposure
In some parotid gland tumors, radiation taken to the head and neck region in the past is shown as the cause. This risk will increase even more, especially if the person is elderly. In this respect, it is important not to give radiation to the head and neck area when it is not needed.
Today, when talking on a mobile phone, the device that emits electromagnetic radiation becomes very close to the parotid gland. Using the mobile phone as little as possible or using a headset may also reduce the risk.
Reduce chemical exposure
Due to their profession, people who work with certain chemicals known to be carcinogenic should work in a protected environment as much as possible. These people mostly work in the chemical industry, mining, plumbing, rubber, or nickel industries.
Reduce alcohol consumption
Although alcohol consumption has an effect on the development of some head and neck cancers. But the role of alcohol in parotid cancers is still unclear. Because the effect of alcohol consumption on parotid tumor development has not yet been confirmed. However, quitting alcohol or limiting its use may reduce the risk. Even the use of alcohol-containing oral care products may be risky in terms of regular and continuous exposure of the mouth to alcohol. Therefore, the use of alcohol-free products (eg, ADA approved mouthwash: TheraBreath Fresh Breath, CloSYS Sensitive Gentle Mint, CloSYS Ultra Sensitive Unflavored, or as a different choice: Tom’s of Maine Natural Wicked Fresh, etc.) is safer.
Live a healthy life
Some studies have found that a diet rich in vitamin C and low in cholesterol can be effective in preventing salivary gland cancer. In this respect, a healthy diet, good immunity, and high morale can be effective in reducing the risk of developing parotid cancer.
References
American Cancer Society: “What’s New in Salivary Gland Cancer Research and Treatment?”
Cedars-Sinai: Health Library, “Salivary Gland Disease and Tumors”
John Hopkins Medicine, Conditions and Diseases, “Salivary Gland Cancer”
Mayo Clinic: Diseases and Conditions, “Salivary gland tumors”
National Center for Biotechnology Information (NCBI): “Parotid Cancer”
NCCN Clinical Practice Guidelines in Oncology: “Head and Neck Cancers, Version 2.2020”