Sublingual Gland Cancer
The sublingual gland is the third-largest salivary gland whose tumors are usually malignant (sublingual gland cancer). The most common sublingual gland cancers are adenoid cystic carcinoma and mucoepidermoid carcinoma. And the most common benign sublingual gland tumor is pleomorphic adenoma.
The causes of sublingual gland tumors are unknown. Risk factors such as exposure to radiation, exposure to chemicals, tobacco use, and alcohol consumption may have an impact on the development of sublingual gland cancer. Due to the frequent absence of symptoms, early diagnosis of most sublingual gland tumors delays. Avoiding risk factors may be beneficial in sublingual gland cancer prevention.
The diagnosis of sublingual gland tumors can be made by biopsy. The survival rate may vary depending on the type, stage, and spread of sublingual gland cancer. In general, the main treatment for sublingual gland tumors is surgery. After surgery, the patient receives radiation therapy, and sometimes chemotherapy.
The Sublingual Gland
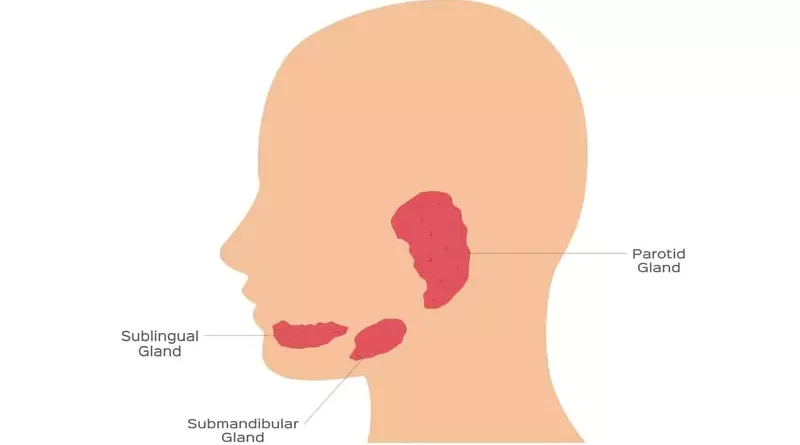
The sublingual gland is the smallest (after the parotid and submandibular glands) major salivary gland and makes the least saliva. Unlike the parotid and submandibular glands, the sublingual gland is unencapsulated. The sublingual gland is located on both sides of the tongue, behind and on the floor of the mouth. Sublingual glands under the tongue empty the saliva they produce into the mouth with multiple ducts.
Sublingual gland tumors are much less common than parotid and submandibular glands. In general, as the size of the salivary gland decreases, the risk of malignancy of the salivary gland tumor increases. Most parotid tumors are benign. Half of the submandibular gland tumors are benign and half are malignant. And, most of the sublingual gland tumors are malignant.
Signs and Symptoms
Sublingual salivary gland tumors develop on the floor of the mouth. Since sublingual gland tumors are often asymptomatic, the patient may not notice for a while. Benign tumors usually grow slowly (over months and years). However, over time, benign sublingual gland tumors can turn into malignant. Malignant sublingual gland tumors develop and spread in a short time (within weeks and months).
We can also see salivary stones (sialolithiasis) blocking the duct of the sublingual gland. Sialolithiasis is a common disease of the salivary glands and occurs mostly in the submandibular gland. However, sialolithiasis of the sublingual gland is very rare. Therefore, it is possible to confuse it with sialolithiasis of the submandibular gland.
Sialolithiasis can cause swelling, redness, and pain in the sublingual gland. These stones can sometimes cause inflammation of the sublingual gland (sialadenitis). In case of inflammation of the sublingual gland, swelling, pain, and redness increase. Antibiotic treatment or movement of the stone provides recovery in the gland. However, the swelling due to the tumor of the sublingual gland does not regress and does not shrink, it progresses further over time.
A submucosal tumor-like lesion in the floor of the mouth may also arise from the submandibular duct or adjacent minor salivary glands. That is why, when a malignant salivary gland tumor exists on the floor of the mouth, it is important to determine whether it originated from the sublingual gland or not.
Swelling in the floor of the mouth on one side
Sublingual gland tumor manifests itself as a swelling, lump, or submucosal mass causing discomfort under the tongue, existing usually for more than 2-3 weeks. In general, the tumors are unremarkable from the outside and no abnormal mass in the face is seen.
The mass in sublingual gland cancer is harder than benign tumors. It is less mobile and more fixed if attached to the surrounding muscles and jawbone. Swollen sublingual salivary glands are usually one-sided.
Subsequent pain in the sublingual area
Typically, a sublingual gland tumor presents as a painless swelling in the floor of the mouth. Pain may occur, especially in association with late-stage malignant tumors. As cancer spreads further into surrounding tissues and nerves, the pain increases more. In these cases, the tumor manifests itself with persistent pain in the tongue and floor of the mouth, affecting speech and mastication. Benign sublingual gland tumors do not invade surrounding tissues and generally, they have a painless course.
Ulceration of overlying mucosa
If the malignant tumor of the sublingual gland is close to the oral mucosa, it may cause mucosal changes, redness, or ulcer formation over time. That is why malignant sublingual gland tumors may present as a submucosal intraoral mass that subsequently ulcerates
Enlarged glands of the neck on one side
Malignant sublingual gland tumors can spread to the lymph nodes in the neck. In this case, they cause swelling in the sides of the neck. In benign submandibular gland tumors, there are no signs such as enlargement of the neck lymph nodes.
Without any symptoms
Sublingual gland tumors are generally asymptomatic until they reach the late stage, mainly because of minimal symptomatology. That is why we notice them incidentally during imaging tests taken for other reasons or during dental examinations. The ability to imitate non-malignant lesions allowing the tumor to grow without specific signs could be responsible for a delay in diagnosis.
Causes
Although tobacco use, radiation exposure, occupational chemical exposures, and sometimes alcohol consumption are considered risk factors for the occurrence of malignant sublingual gland tumors, there is no clear scientific evidence. It is also unclear whether sublingual salivary gland tumors are linked to viruses, diet, or other factors. In particular, the causes of benign tumors of the sublingual gland are more unclear.
Risk Factors
Gender distribution is equal for sublingual salivary gland tumors. Most cases occur in the fifth decade. Sublingual salivary gland tumors can develop at any age, including childhood. Benign sublingual gland tumors are more common in the young and middle age group, and malignant tumors are generally more common in older people.
Being older
The median age of patients with malignant sublingual gland tumors is fifty years. Although tumors can occur at any age, malignant tumors are most common in older adults.
Tobacco use
Tobacco use is a serious risk factor for mouth and throat cancers. In this respect, it is possible that sublingual gland tumors, especially malignant tumors, may also be associated with smoking. Because tobacco use is common in patients. Apart from this, tobacco use is also a risk factor for benign sublingual tumors to become malignant.
Exposure to radiation
Radiation exposure, including radiation therapy, is a risk factor for sublingual salivary gland cancer. Mobile phones also affect the salivary glands with electromagnetic radiation. Today, some doubts focus on the electromagnetic effect of the phone. But there is no proven fact yet.
Exposure to chemicals
Sublingual gland cancer risk may increase in people who work with certain substances. The chemical industry, mining, rubber, or nickel industries are among the risky jobs in terms of salivary gland cancers. Regular occupational exposures to carcinogenic substances have a great influence in this respect.
Alcohol consumption
Alcohol consumption is a risk factor for various mouth and throat cancers. However, the role of alcohol in the development of salivary gland tumors is unclear. There is no evidence of the effect of alcohol consumption on the development of sublingual gland tumors.
Types of Tumors
The tumor is a term that refers to the masses that cells form by uncontrolled proliferation. Tumors can develop from any tissue in the body, including the salivary glands. Tumors are generally benign or malignant. Most sublingual salivary gland tumors are malignant. Malignant tumors of the sublingual gland are sublingual gland cancer.
Benign sublingual gland tumors
Benign tumors of the sublingual salivary gland grow slowly. This growth occurs over months, even years. They do not metastasize to surrounding tissues or distant organs. Most benign sublingual gland tumors are encapsulated. These tumors generally do not invade surrounding tissues. They usually grow by pushing the surrounding tissues. The most common benign sublingual gland tumors are the following;
Pleomorphic adenoma (benign mixed tumor)
Pleomorphic adenoma is the most common benign sublingual gland tumor. Although it is most common in the parotid gland, it can also develop from the sublingual salivary gland.
If the surgeon doesn’t remove completely the pleomorphic adenoma of the sublingual gland, it can turn into a malignant tumor over the years. In this case, the mass in the floor of the mouth, which has existed for years and grows very slowly, begins to grow rapidly. One-tenth of pleomorphic adenomas that have existed for more than 15 years can become cancerous.
Basal cell adenoma
Basal cell adenoma is a benign tumor and mostly arises from the parotid gland. However, this tumor can also develop from the sublingual gland.
Oncocytoma
Oncocytoma is a benign tumor that mostly originates from the parotid gland. However, oncocytoma can also develop from the sublingual salivary gland. These tumors arise from a type of salivary gland cell called oncocyte.
Other benign tumors
Although rare, benign tumors such as canalicular adenoma, myoepithelioma, and sialoadenoma papilliferum may develop from the sublingual salivary gland. There may also be masses of the sublingual gland originating from vessels such as hemangioma, lymphangioma, and salivary gland cysts.
Malignant sublingual gland tumors
Malignant sublingual gland tumors develop and spread rapidly. These tumors can metastasize to neck lymph nodes, lungs, liver, brain, bone, and other areas. Usually, they are not encapsulated. They invade surrounding tissues and disrupt their functions as they grow.
Sublingual gland tumors with low malignancy potential are relatively common in childhood and young adults. The most common malignant sublingual gland tumors are the following;
Adenoid cystic carcinoma
Adenoid cystic carcinoma is the most common malignant sublingual gland tumor. It is more common in people of middle age and older.
Adenoid cystic carcinoma invades nerve fibers in its area and uses them as a way to spread. It spreads with blood and nerve fibers rather than lymph. Adenoid cystic carcinoma can recur even years after surgery and radiation therapy. Lung metastases of adenoid cystic carcinomas are common.
Mucoepidermoid carcinoma
Mucoepidermoid carcinoma is another of the most common malignant sublingual gland tumors. Along with the relatively slow-growing types, there are also types with faster progress and poor prognosis. The patients are generally middle-aged and older adults. However, we can see the mucoepidermoid carcinoma of the sublingual gland in younger people also.
Adenocarcinoma
Adenocarcinomas can also frequently develop from the sublingual gland. Adenocarcinoma of the sublingual gland has types with low malignancy potential, such as acinic cell carcinoma. However, types with high malignancy potential such as oncocytic carcinoma and salivary duct carcinoma are also seen. These types are likely to have an aggressive course and have a less positive outlook.
Malignant mixed tumors
Malignant mixed tumors of the sublingual salivary gland are generally specific to elderly people. Carcinoma ex pleomorphic adenoma is the most common type of these. However, carcinoma ex pleomorphic adenoma of the sublingual gland is extremely rare. Carcinoma ex pleomorphic adenoma is the untreated pleomorphic adenoma that has transformed into a malignant tumor after many years.
Carcinoma ex pleomorphic adenoma is a highly aggressive tumor. When recurrence and distant metastasis occur, there are very low cure rates regardless of treatment. Therefore, early and complete removal of that carcinoma ex pleomorphic adenoma is extremely important.
Acinic cell carcinoma
Acinic cell carcinoma accounts for approximately one-tenth of malignant salivary gland tumors. It often develops from the parotid salivary gland, but we can see it also in the sublingual gland. Acinic cell carcinoma is a tumor with low malignancy potential and grows slowly. Although malignant, they are encapsulated tumors and are unlikely to spread to distant organs.
Acinic cell carcinomas, which we mostly see it in young adults, have a more benign course compared to other sublingual gland cancers. Acinic cell carcinoma can also be seen in children and elderly people.
Other rare cancers
Squamous cell carcinoma, Non-Hodgkin lymphoma, and other cancers can also develop from the sublingual salivary glands. Squamous cell carcinoma occurs mainly in older people. It may develop after radiation therapy which the patient recieves to the jaw area and tends to have a poorer outlook.
Occasionally, Non-Hodgkin lymphomas can start from immune system cells in the sublingual salivary glands. Non-Hodgkin lymphomas that start in the salivary glands affect people with Sjögren’s syndrome. Non-Hodgkin lymphomas can develop from both sublingual glands at the same time.
Diagnosis
A patient who suspects sublingual salivary gland cancer should first consult an otolaryngologist (ear, nose, and throat doctor). The diagnosis process begins when the patient notices a swelling, mass, or ulcer on the floor of the mouth area and consults a doctor. The doctor first listens to the patient’s complaints. Next, the doctor asks the patient various questions about the symptoms. Then the examination phase starts.
Physical exam
An otolaryngologist examines the patient in a general ear, nose, mouth, throat, and neck. The doctor carefully examines the lesion in the floor of the mouth area in terms of size, hardness, mobility, adhesion to surrounding tissues. Next, the doctor checks for weakness reduced movement, or sensory perception of the tongue.
Removing a tissue sample
Taking a cell or tissue sample from the mass in the sublingual gland is necessary to confirm the diagnosis and plan the treatment. Since the tumor of the sublingual gland is usually associated with the inside of the mouth, the doctor takes tissue samples from the tumor by incision. Taking tissue samples from the tumor, the doctor performs under local anesthesia so that the patient does not feel pain.
If the tumor has developed as a swelling closer to the skin and the mass does not have a relationship with the oral cavity, it is safe to take tissue samples with a fine needle biopsy. Therefore, in cases where the tumor is located under the oral mucosa, the doctor takes tissue samples from the mouth by incision. The pathologist examines the cell and tissue samples taken from the sublingual gland with biopsy and reports the result to the surgeon.
Sometimes the surgeon skips the biopsy, which gives preliminary information about the type of sublingual gland tumor, and surgically removes the entire tumor. The pathologist examines the tumor removed by the surgeon in detail and thus reaches the final diagnosis. So, it can be that the diagnosis made with the biopsy before the surgery can change with the examination of the removed tumor by the pathologist.
Imaging tests
Performing imaging tests for salivary gland tumors associated with the mouth is usually after taking tissue samples from the tumor. A doctor who suspects a sublingual salivary gland tumor by examination usually needs one or more imaging tests such as ultrasonography (USG), magnetic resonance imaging (MRI), or computed tomography (CT). Ultrasonography (USG) is often the first imaging test used.
MRI imaging gives much more information about soft tissues and their properties compared to CT. Accordingly, MRI with intravenous medication (contrast agent) has become almost a standard in terms of examining the salivary gland tumor. Computed tomography (CT) can also allow examining many features related to the mass in the sublingual gland in detail. The radiologist interprets the imaging tests and reports them to the surgeon.
Imaging tests are procedures that help diagnose sublingual gland tumors. Benign tumors of the sublingual salivary gland are well-bordered on MRI or CT and do not occupy the surrounding tissues. Malignant sublingual gland tumors, on the other hand, often appear to occupy the surrounding tissues depending on their location and whose borders cannot be clearly identified.
Adenoid cystic carcinoma of the sublingual gland, which is at risk of spreading to distant organs such as the lungs, requires imaging tests such as positron emission tomography (PET) and lung CT. These imaging tests are ideal for revealing whether there is metastasis.
Treatment
The main treatment of all sublingual salivary gland tumors, regardless of whether they are benign or malign, is the surgical removal of the tumor. Because benign sublingual gland tumors will also continue to grow over time and make the treatment more difficult. Apart from this, there is also the possibility that a benign sublingual gland tumor can turn into a malignant tumor over time. In addition, there are transition zone tumors of the sublingual gland that are not clear they are malignant or benign.
The surgeon usually removes the tumor with sublingual gland. If the surgeon has completely removed the tumor along with the sublingual gland and the pathology examination shows that the tumor is benign, the treatment is complete. In these cases, the patient does not receive additional treatments after surgery, such as radiation therapy and chemotherapy. Radiation therapy and chemotherapy are not required in the treatment of benign sublingual gland tumors, with exceptions.
After the complete removal of malignant sublingual gland tumors from the body, the patient may receive radiation therapy and sometimes chemotherapy. Additional treatments are usually applied after surgery for sublingual gland tumors with high malignancy potential. However, if the patient’s health condition is not suitable for surgery or if the malignant tumor has spread to the extent that the surgeon cannot remove it by surgery, other treatment options may come to the fore without surgery.
Treating doctors
Problems in the floor of the mouth caused by the sublingual salivary gland mainly belong to the field of otolaryngologists. Otorhinolaryngologists experienced in head and neck surgery or oral and maxillofacial surgeons perform surgeries related to sublingual salivary gland tumors. Radiologists, radiation oncologists, medical oncologists, dentists, and psychologists can also participate in the diagnosis and treatment process of sublingual gland tumors.
Surgery
Sublingual salivary gland tumor surgery is almost always performed under general anesthesia and generally via an intraoral approach. This often means that there is no external surgical incision. However, surgery may vary depending on the location of the tumor in the salivary gland.
During the surgery of the sublingual salivary gland tumor, the hypoglossal nerve that moves the tongue and the lingual nerve that provides the tongue’s taste and touch sense are in the foreground.
Tumor removal
The tumor of the sublingual gland located on the floor of the mouth is usually treated by removing it completely along with the salivary gland. Depending on the tumor size and location, the total resection may become quite complex. Because some malignancies are maybe very close to the inner side of the lower jaw, the submandibular salivary gland and its duct, the lingual vessels, the lingual, and the hypoglossal nerves.
Lymph node removal
While the surgeon removes the malignant tumor of the sublingual gland, he also removes the neck lymph nodes with the highest probability of the tumor spreading. We call this is a neck dissection. Neck dissection is a standard treatment for many malignant tumors located in the face, head, and neck regions. The surgeon usually performs the neck dissection in case of lymph node metastasis detected by examination or imaging tests in the neck. However, even when there is no metastasis insight, the surgeon can also perform this procedure to prevent future metastases.
The surgeon usually performs the neck dissection during the same surgical session in which the malignant sublingual gland tumor is removed. If the pathologist diagnosed sublingual gland cancer in the pathological examinations of the tumor after surgery, the surgeon removes the neck lymph nodes of the same side with a second operation. The surgeon may not prefer neck dissection for sublingual gland tumors with low malignancy potential. There is no need for neck dissection surgery for benign sublingual gland tumors.
Reconstruction
After removing the sublingual gland tumor, the surgeon proceeds to the repair phase. The surgeon mainly tries to make repairs that provide tongue and jaw movements.
During surgery, the surgeon can remove muscle, nerve, or bone tissue from the area along with the tumor. If the surrounding tissues are not sufficient for the repair, the surgeon can transfer muscle, nerve, or bone tissue from other parts of the body to repair the tongue or jaw.
Normalization after surgery
The patient undergoing surgery for a sublingual salivary gland tumor usually stays in the hospital for a few days. After surgery, the patient carries the tube called the drain for a few days to remove the blood and fluid accumulation from the surgical wound.
After sublingual salivary gland surgery, the patient may need pain relievers. Pain relievers are often sufficient to deal with pain. Antibiotics are given to the patient for a few days against infection. Apart from these, after the surgery, swelling of the face and neck may occur as a result of blood and fluid accumulation. With the doctor’s intervention, these situations pass without causing a problem.
Radiation therapy
The radiation oncologist applies the radiation produced by special devices to the tumor area and the areas where the tumor is likely to spread. Radiation therapy is an additional treatment applied after tumor surgery and aims to increase the patient’s chance of getting rid of cancer. Radiotherapy is not the sole or main treatment for sublingual salivary gland cancers.
Radiation therapy is the treatment for malignant sublingual gland tumors. Sublingual gland tumors with intermediate and high malignancy potential require radiation therapy after complete surgical removal of the tumor. But very rarely, persistent benign sublingual gland tumors may also require radiation therapy.
Chemotherapy
Chemotherapy uses anti-cancer drugs, which kill cancer cells in the body. However, chemotherapy has no place in the standard treatment of sublingual salivary gland cancers. Treatment with medication alone will not work unless there is an inflammation-like condition in the sublingual gland.
Chemotherapy is mainly applied in the treatment of lymphoma of the sublingual gland. For other cancers of the sublingual gland, the benefit of chemotherapy is limited. Chemotherapy may have a place in the treatment of sublingual gland cancers in the presence of metastasis, or when the complete removal of the tumor is impossible or the tumor recurs. Medical oncologists apply chemotherapy.
Targeted therapy
No targeted therapy drug has so far been effective in salivary gland cancers, including the sublingual salivary gland. Targeted therapy research for salivary gland cancers is still at an early stage.
Nerve functions after surgery
In cases where the sublingual gland tumor affects the hypoglossal or lingual nerves, patients may already have numbness and weakness to a certain extent before the surgery. In cases where the sublingual gland cancer has damaged the nerves, this weakness can progress to impairment of movement or paralysis of the tongue.
If the tumor has not damaged the nerves very seriously, problems with the tongue can usually resolve within weeks after surgery. In cases where the tumor has severely damaged the nerves, the surgeon repairs it with a nerve graft taken from another part of the body. However, even in experienced hands, these nerves rarely fully recover functionally.
Salivary functions after surgery
Three pairs of major and many minor salivary glands open into our mouths through various channels. The surgeon’s removal of one of these glands due to a tumor does not cause a decrease in the amount of saliva in the mouth. In particular, the sublingual gland is the smallest of the major salivary glands and secretes the least saliva. Other salivary glands take over the function of this small salivary gland without any problems. However, if the patient has received radiation therapy after surgery, there may be dry mouth problems for a while. In these cases, ADA approved dry mouth mouthwash (eg, Biotene Dry Mouth Oral Rinse, or as a different choice: TheraBreath Dry Mouth Oral Rinse, etc.) may be beneficial for the patient.
Speaking and feeding after surgery
After sublingual gland tumor surgery, the patient is not given liquid or food orally until the effect of anesthesia disappears. Initially, the patient feeds intravenously or by a tube that is extended from the mouth to the stomach, then gradually switches to soft foods and normal foods. After extensive surgeries due to large tumors, it may take a while for the patient to return to their normal diet. However, unless there are interventions such as removing the tongue or jawbone, functions such as nutrition and speaking are not permanently affected.
Saliva helps digestion by keeping the mouth and throat moist. In addition, saliva creates a defense mechanism against microorganisms that cause infections in the mouth and throat. Therefore, due to the side effects of radiation therapy that reduce saliva secretion, sores may occur in areas such as the mouth and throat. These problems may cause speaking and swallowing difficulties for a while. However, these problems also pass over time.
Prognosis
Generally, if sublingual salivary gland cancer is found early and treated, the prognosis is good. Overall, the prognosis for salivary gland cancers is better for children and adolescents. The main reasons for this are the lower frequency of metastasis, less local soft tissue spread, and relatively different types of cancer. Overall survival for children after treatment is better than for adults.
The prognosis depends mainly on the type of the tumor, the stage at presentation, and adequate primary surgical and additional treatment as radiation therapy.
Regardless of the type of malignant sublingual gland tumor, adverse prognostic factors for survival, are older age, advanced stage of cancer, presence of distant metastasis, presence of pain, and comorbidities. In sublingual gland cancers, distant metastases most often occur to the lungs, bone, liver, and brain. Distant metastases are the main cause of death in sublingual gland cancers.
Follow-up care
Regular medical check-ups after cancer treatment have two main goals. The first goal is to detect recurrence after cancer treatment. And second is to manage any treatment complications that may arise. Long-term follow-up is very important for sublingual gland cancers. Most recurrences of sublingual salivary gland cancers occur in the first 3 years after treatment. Patients should receive follow-up at regular intervals within 5 years after treatment. The patient should continue to receive regular follow-up every 1 year thereafter.
All salivary gland tumors, including sublingual gland tumors, require observation for up to 20 years after treatment. In particular, the follow-up of adenoid cystic carcinoma is important because of its delayed recurrence and tendency to metastasis. Annual chest screening is required for tumors with high malignancy potential due to the high risk of pulmonary metastasis. Patients who receive radiation to the neck area should have their thyroid hormone levels checked several times a year.
Recurrence of cancer
Generally, half of the malignant salivary gland tumors recur after initial treatment. In this respect, sublingual gland tumors may also recur after treatment. In these cases, if possible, the surgeon attempts to remove the tumor and the surrounding tissues completely with repeat surgery. However, if the cancer of the sublingual gland recurs, the repeat operations to be performed will be more difficult than the first operation. Because it will not be easy to recognize and protect important structures such as nerves in the region due to the healing tissues caused by the previous surgery.
Prevention
The cause of malignant sublingual gland tumors is unknown. Information on the causes of benign tumors of the sublingual gland is much less. In this respect, ways to prevent tumors of unknown origin are not clear either. However, avoiding certain things can be beneficial in preventing sublingual gland cancer.
Quit smoking
Tobacco use is a risk factor for sublingual gland cancers, as it exposes the mouth and throat to certain carcinogenic substances. Especially if the person is older, this risk will increase even more. In general, it is thought that avoiding tobacco can reduce the risk of sublingual gland tumors.
Reduce radiation exposure
Even if it is for treatment purposes, radiation is taken to the mouth and jaw area in the past (especially during dental treatments) may trigger the development of sublingual gland tumors. Old age will increase this risk even more. In this respect, avoiding exposure to radiation to the mouth, under the chin, and neck area when it is not needed may reduce the risk of sublingual gland cancer. Due to the electromagnetic radiation it emits, using a mobile phone as little as possible or using it with a headset may also reduce the risk.
Reduce chemical exposure
Because of their profession, people who work with some carcinogenic chemicals should work in a protected environment as much as possible. These people mostly work in the chemical industry, mining, plumbing, rubber, or nickel industries.
Reduce alcohol consumption
It is known that alcohol consumption has an effect on the formation of some mouth and throat cancers. However, the effect of alcohol on the development of sublingual salivary gland tumors is not yet clear. However, quitting alcohol or limiting its use can reduce the risk. Even the use of alcohol-free oral care products reduces the risk. Because by using the alcohol-containing ones we regularly and continuously expose the mouth to alcohol. In this respect, the use of alcohol-free products (eg, ADA approved mouthwash: TheraBreath Fresh Breath, CloSYS Sensitive Gentle Mint, CloSYS Ultra Sensitive Unflavored, or as a different choice: Tom’s of Maine Natural Wicked Fresh, etc.) is very important.
Get regular dental checkups
Dentists, often first detect sublingual gland cancers during regular dental checkups. Therefore, regular examination of the dentist is important to detect these cancers at an early stage.
Live a healthy life
A healthy diet, good immunity, and high morale are important to reduce the risk of developing salivary gland cancer, including sublingual gland cancer. Some studies have found that a diet rich in vitamin C and low in cholesterol can be effective in preventing salivary gland cancer.
References
American Cancer Society: “What’s New in Salivary Gland Cancer Research and Treatment?”
International Journal of Oral Science (IJOS): “ Carcinoma ex pleomorphic adenoma of the sublingual gland: a case report”
Mayo Clinic: Diseases and Conditions, “Salivary gland tumors”
National Center for Biotechnology Information (NCBI): “Adenocarcinoma of the sublingual salivary gland – A case report”
NCCN Clinical Practice Guidelines in Oncology: “Head and Neck Cancers, Version 2.2020”
ResearchGate: “Tumors of the sublingual gland: a national clinicopathologic study of 29 cases”